A retrospective evaluation of cerebrospinal meningitis data in upper West Region, Ghana, 2015-2021
Joseph Kwame Wulifan, Frederick Dapilah, William Angko
Corresponding author: William Angko, Departments of Economics, Faculty of Social Science and Arts, Simon Diedong Dombo University of Business and Integrated Development Studies, Bamahu, Ghana 
Received: 05 May 2022 - Accepted: 13 Jul 2022 - Published: 20 Jul 2022
Domain: Epidemiology, Health Research, Public health
Keywords: Cerebrospinal meningitis, case fatality rate, surveillance data, Upper West Region
©Joseph Kwame Wulifan et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Joseph Kwame Wulifan et al. A retrospective evaluation of cerebrospinal meningitis data in upper West Region, Ghana, 2015-2021. PAMJ-One Health. 2022;8:13. [doi: 10.11604/pamj-oh.2022.8.13.35310]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/8/13/full
Program evaluation 
A retrospective evaluation of cerebrospinal meningitis data in upper West Region, Ghana, 2015-2021
A retrospective evaluation of cerebrospinal meningitis data in upper West Region, Ghana, 2015-2021
&Corresponding author
Cerebrospinal meningitis (CSM) is a disease of public health concern for countries within the Sahel region and Ghana. The Upper West Region has been recording CSM cases over the years. This study seeks to generate evidence using CSM data from the region to make recommendations to improve surveillance. To establish evidence to improve surveillance, we pooled CSM surveillance dataset from 2015 to 2021 for all the 11 districts/municipalities in the region. The study employed retrospective descriptive cross-sectional review design using both univariate and bivariate analysis. A total of 2,066 cases within the study period were reported. Out of these cases, 50.82% (1,050/2,066) were males while the remaining 49.18% were females. The proportion of reported cases aged 0 to 29 years was 65.34%. The Overall Case Fatality Rate (CFR) was 10.8% (233/2,066). In all, 74% of the cases were recorded between January and April. Laboratory confirmed cases were 18%. The result further showed that 17% (X2 = 18.69; P < 0.000) of these laboratory-confirmed cases died. Also, 8% of the negative cases and 10% of laboratory suspected cases died.. Most CSM cases were recorded in the dry season with most victims being persons younger than 30 years. Almost a quarter of the cases were laboratory confirmed and the most recent year witness a decline in morbidity and mortality rates. There is need to take note of these trends and intensify CSM surveillance to improve on the laboratory confirmed cases.
The prevalence of cerebrospinal meningitis (CSM) within the Sahel regions is a significant public health concern [1-3]. Meningitis outbreak is commonly caused by infectious pathogenic organisms such as fungi, bacteria, parasites, rickettsia and viruses, with the most common strain being from the bacteria types called Neisseria Meningitis, Streptococcus pneumonia and Haemophilus influenza type B [2,4,5]. Neisseria Meningitis remains the leading cause of fatal sepsis within the Sahel belt in recent times [4]. Meningococcal disease is caused by bacteria called Neisseria meningitides. People with meningococcal disease spread the bacteria to others through close personal contact such as living together or kissing each other. A person with meningococcal disease needs immediate medical attention [5-8]. Meningococcal Meningitis is endemic in the Sahel belt in sub-Saharan Africa, stretching from Ethiopia to the east of Africa through to Chad and South Sudan in Central Africa to Northern parts of Nigeria, Togo, Ghana, Burkina Faso, south of Mali, Senegal, Gambia, Guinea-Bissau and Guinea [1,4,5]. Given the porous nature of African borders, there is a high tendency of CSM outbreaks spreading from one country to the other [2,9,10]. The symptoms of meningococcal disease can vary based on the type of illness. Common symptoms of meningococcal meningitis include sudden fever, headache, photophobia and stiff neck [4,5]. Other symptoms may include nausea, vomiting, increased sensitivity to light, and convulsion. Children and infants may show different signs and symptoms, such as inactivity, irritability, vomiting, or poor reflexes. Bacteria that cause meningococcal disease can also infect the blood, causing septicemia. Symptoms of septicemia include tiredness, vomiting, chills, severe aches and pain, fast breathing, diarrhea, and a dark rash. Meningococcal disease can lead to death in as little as a few hours [2,4,5,10-13].
The historical evidence of CSM epidemic outbreaks occurs annually mostly during the dry season in this sub-Saharan meningitis belt of Africa (November-May) with incidence rates ranging from 10 < x < 1,000/10,000 persons and a case-fatality rate of about 10% [4,5,7,12,14,15]. In Ghana, Institutional CFRs are between 36% < x < 50% with about 10% to 20% of persons who recover from this CSM suffering from neurological complication which include hearing impairment, mental retardation and epilepsy [3,5-7,9,12]. The burden of CSM in Ghana cannot be underestimated, particularly within the regions that lie within the northern part of Ghana. For instance, from 2010 to 2015 a total of 1,176 suspected meningitis cases were recorded in 26 districts in the then Northern region, of which males accounted for 53.% (629/1,176) [5]. Also in the 2016 outbreak in Ghana, of the 59 affected districts, a total of 2,184 confirmed cases of meningitis were recorded with the then Brong Ahafo region recording the highest figure of 974 cases [2,16]. The Northern region which shares boundary with the Upper West region recorded extremely higher cases in 2014 with focal epicenters of the epidemic in Yendi Municipality with a CFR of 6.02% (5/83) [5,17]. Ghana was hit by many meningococcal meningitis from strain A and C before 2010. In 2010 the Upper West region was hit by the first epidemic caused by W135, this was followed by a second strain in the Upper East region in 2012. The CFRs were 17.9% and 17.3% respectively [5,18,19]. It is against this background that we seek to review the recent 7-years Meningitis surveillance data in the Upper West region 2015 - 2021 to describe the disease occurrence trend to improve CSM surveillance in the region.
Study area: The Upper West Region of Ghana is located in the North-western corner of Ghana and is bordered by Upper East region to the east, the Northern region to the south, and Burkina Faso to the west and north. Wa, the regional capital, is the largest settlement in the Upper West Region. The region lies on between latitude 9.8° - 11.0° North and longitude 1.6°- 3° West. It covers a geographical area of 18,476 square kilometers, representing 12.7% of the total land area of Ghana. It is the seventh-largest region in Ghana in total area, and it is made up of 11 districts. There are a total of 448 health facilities providing various types of health services in the region. The facilities comprise three (3) district government hospitals, one (1) regional hospital, two (2) CHAG hospitals and three (3) private hospitals. The rest are five (4) Polyclinics, 72 health centres, 10 clinics, 5 maternity homes and 319 CHPS Compounds. Two out of the nine districts in the region (Wa East, and Lambussie) have no district or private hospital. The climate of the region is tropical continental with temperature ranging from 15°C to a high 40°C during the hot dry season. The region has a single maxima of rainfall. The rains begin in drizzles in April and increases steadily to its peaks in August/September and then drop by October. The dry season takes off from November to March with the North East trade winds (Harmattan winds) virtually dominating the entire period (November - March) these conditions enable the CSM to thrive in epidemic proportions in the region. By virtue of the regions' location, the Upper West Region has the potential for international and inter-regional trade and other bi-lateral relations, but the overspill of criminal activities and disaster, such as bush fires, diseases and pestilence, armed robbery etc., from the region's neighbors also pose a threat [19-21].
Study population: the 2021 population and Housing census put the region´s population at 901,502 people at a growth rate of 2.4% per annum. In the Upper West Region, females form 51.16% (461,185/901,502) as against their male counterparts being 48.84% (440,317/901,502). This population forms 2.9% of the population of Ghana, with a population density of about 49.79 per square kilometer. About 74% (663,218/901,502) live in rural areas, with approximately 74% and 73% each being males and females respectively. Settlements in the rural areas are dispersed, hence having implication for service delivery as Sub-District health Teams would have to travel to rural settlements for out-reach services [20].
Study design: a retrospective descriptive study was employed to review the CSM surveillance dataset from January 2015 to December 2021. We retrieved an electronic version of the CSM surveillance datasets captured as line lists in MS-Excel spreadsheets. Important Socio-demographic characteristic of clients that were extracted where age, sex, district/municipal, date of birth, date of onset of ailment, date reported at the facility, facility type, epi-weeks cases were reported, final Laboratory classification of the test results, type of CSM and outcome of ailment. We coded data using MS-Excel, then we imported the MS-Excel file into Stata software for analysis. The analysis was executed using person (age and sex), place (district/municipal), time (epi-month and epi-year), causative organism identified, final laboratory classification of test results (negative, confirmed and suspected) and outcome of the ailment (died and alive). Outputs of the univariate and bivariate analyses were represented in graphs and tables in proportions and percentages.
Ethical consideration: to ensure confidentiality, patients identifiers were deleted, and we also sought permission from Ghana Health Service.
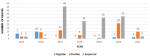
Univariate: a total of 2,066 CSM cases were report from all 11 districts/municipals for the 7-year period (2015-2021) under review. The general numbers and trend of the disease burden is shown in Table 1, Table 2. The results showed that males represented 50.82% (1,050/2,066) of the reported cases. Reported cases for children 0-4 years constituted 17.76% (367/2,066) while the proportion of cases 0 - 29 years constituted 65.34% (1,350/2,066) and those 65 years and above were 7.12% (147/2,066). From the final laboratory results classification all the reported cases, 12.78 % (264/2,066) tested negative, 17.96% (371/2,066) tested positive for CSM (confirmed cases), while 69.26% (1,431/2,066) cases were neither negative nor positive hence classified as suspected. Within the period, the highest reported cases were 20.57% (425/2,066) recorded in the year 2017 followed by 19.99% (413/2,066) cases, reported in 2020. The year with the least was 6.97% (144/2,066), cases recorded in 2016. Nandom municipal recorded the highest number of cases 29.62% (621/2,066) followed by Nadowli-Kaleo district, 20.18% (417/2,066) with the least from Wa East and Sissala West recording less than 0.4% (7/2,066) each. The highest recorded cases were January, February and March representing 15.1%, 22.27% and 27.20% (312, 460 and 562/2,066) respectively. The final outcome of reported cases show that 10.79% (233/2,066) died while 89.21% (1,843/2,066) survived. These are shown in Figure 1, Figure 2.
Bivariate: of the total of 223 meningitis deaths, age 0 - 29, 30 - 64 and above 65 represented 9.33%, 12.30% and 18.37% (X2 = 13.09; P < 0.001) respectively. Males and females who died due to meningitis cases were 12.67% and 8.86% (X2 = 7.78; P < 0.005) respectively. Of the final laboratory classification and meningitis deaths, the negative, positive (confirmed) and suspected cases each recorded 7.95%, 16.98% and 9.71% (X2 = 18.70; P < 0.000) respectively. The highest meningitis deaths of approximately 14% each were recorded in 2016, 2017 and 2020 with the months December and May each also recording the highest meningitis death (25.00% and 15.32%). This is shown in Table 3.
From the reviewed data, the CSM disease burden in the Upper West Region is unevenly distributed by person age, place (districts/municipals), time (epi-month and epi-year) and laboratory results classification. Distribution by sex is nearly equal. The most common pathogen is streptococcus pneumonia. Our results, as presented, are consistent with documented epidemiological evidence along the sub-Saharan Sahel CSM belt [2,4-6]. The CFR rose steadily from 7%) in 2015 to 14% in 2017, then drops to 8% in 2018 thereafter rose again in 2019 to nearly 2 folds (14%) in 2020. This rise of more than 10% in CFR is consistent with figures quoted from developing countries and particularly those within the CSM Sahel belt [2,5,9,12,22]. These modest gains in the drop in the CFR to below 10% can be attributed to strenuous efforts of investment made by successive governments within the period to provide timely vaccines to the region to combat the spread of CSM cases [2-4,10,19]. Consistent with literature, rigorous public awareness education on the CSM epidemics, improve literacy rate in communities, improvement in moderate ventilated housing and awareness of avoiding overcrowding could all be plausible reasons for the decline in CFR in 2015 and 2021 in the Upper West Region [13,22,23]. Also, females in the region form 51.16% as against their male counterparts 48.84% however the findings suggest that 51% of males contracted CSM within the period which is similar to another five year evaluative study conducted in Northern region from 2010 to 2015 [5]. Two studies in 2000 and 2006 respectively found prevalence of CSM among males compared to their female counterparts [24,25].
Streptococcus pneumonia was identified as the dominant pathogen, with the highest cases occurring in 2020. This finding confirms a similar retrospective study conducted in 2010 to determine how the outcome of bacterial meningitis in children is influenced by the identity and antibiotic susceptibility of the causative pathogens [26]. The uneven distribution of the meningitis incidence across the region is overt in the Nandom municipal, closely followed by Nadowli-Kaleo district and Jirapa municipal. Nandom municipal recorded a third of the cases and this could be attributed to the area been located in the Sahel belt and also as a border town which is often prone overspill of disease due to its closeness to the international border. That apart, the hot, dry, dusty winds conditions during the day in the dry season equally increases the risk of communicable diseases as inhabitants are often tempered to shut their windows resulting in poor ventilation and overcrowding which facilities transmission of CSM consistent to 2 studies in literature [5,26]. The study identified some few incomplete details which could be attributed to inadequacy of laboratory services in the region in terms of laboratory infrastructure, logistics and critical staff in adequate proportions. Effective clinical case management is dependent on the confirmation of specific causative pathogens among cases at the laboratory [2,5,11,23].
Limitation of the study: the CSM surveillance dataset retried were based on reported cases at each facility, which may not be accurate representative of the cases and distribution of CSM cases across all the 11 districts/municipals in the Upper West Region of Ghana.
The dry season witnessed the highest reported case of CSM in Upper West Region for the period January 2015 to December 2021 as well as among the age group younger than 30 years. Males recorded a slightly higher incidence of CSM cases compared to their female counterparts. There is uneven burden of CSM distribution across the districts/municipalities with Nandom municipal which is around the international borders being the highest. The CFR of SCM for the period rises and falls within the period. The laboratory surveillance data showed incomplete records in some scenario, hence the findings suggest the need for accurate surveillance records for better diagnosis services to reduce the morbidity and mortality trend of SCM in the Upper West Region.
What is known about this topic
- CSM is a disease of public health concern as Upper West Region falls within the CSM Sahel belt;
- There has been annual CSM case outbreaks in the region over the past half century;
- North-western part of Ghana is one of the CSM endemic regions.
What this study adds
- Incomplete laboratory records which needs to be worked on so as to improve the surveillance system to enhance CSM case management in the Upper West Region;
- Border towns are potential for CSM outbreak hence cross border surveillance and health system strengthening along border towns should be enhanced;
- The most dominant bacteria strain among confirmed cases was Streptococcus pneumonia
The authors declare no competing interests.
JKW, FD and WA conceptualized the idea. Data extraction was done by JKW, FD and WA, Data cleaning and analysis were executed by JKW, FD and WA. Draft of script was carried out by JKW. Review was done by FD and WA. All authors read through and finalized the draft for submission.
We acknowledge the Disease Control Department for Upper West Regional health Directorate for the Data. We are also grateful to Lawra Municipal Health Director for the support he gave to the authors.
Table 1: estimated CSM cases in Upper West Region (2015-2021)
Table 2: univariate and bivariate descriptive statistics
Table 3: bivariate analysis for risk factors in relation to meningitis
Figure 1: trend of CSM morbidity and mortality cases in Upper West Region (2015-2021)
Figure 2: trend of deaths from cases in Upper West Region (2015-2021)
- Christensen H, Hickman M, Edmunds WJ, Trotter CL. Introducing vaccination against serogroup B meningococcal disease: an economic and mathematical modelling study of potential impact. Vaccine. 2013;31(23):2638-2646. PubMed | Google Scholar
- Dartey B, Afreh O, Teviu E, Khumalo G, Letsa T, Issah K et al. Analysis of meningitis outbreak data, Jaman North District, Brong Ahafo Region, Ghana. Ghana Med J. 2020;54(2):53-58. PubMed | Google Scholar
- Tacon CL, Flower O. Diagnosis and management of bacterial meningitis in the paediatric population: a review. Emerg Med Int. 2012;2012:320309. PubMed | Google Scholar
- Anaseba D, Pelzman J, Pandya R, Hodgson A, Hayden MH, Dalaba M et al. Knowledge, attitudes, and practices related to meningitis in Northern Ghana. Am J Trop Med Hyg. 2013;89(2):265-270. PubMed | Google Scholar
- Kaburi BB, Kubio C, Kenu E, Ameme DK, Mahama JY, Sackey SO et al. Evaluation of bacterial meningitis surveillance data of the northern region, Ghana. Pan Afr Med J. 2017;30(27):1-9. PubMed | Google Scholar
- Butler JC, Tuomanen EI, Mitchell TJ, Morrison D, Spratt BG. The pneumococcus: epidemiology, microbiology, and pathogenesis. Washington, DC, USA: ASM Press. 2014;7(3):148-168. Google Scholar
- Greenwood BM, Greenwood AM, Bradley AK, Williams K, Hassan-King M, Shenton FC et al. Factors influencing susceptibility to meningococcal disease during an epidemic in The Gambia, West Africa. J Infect. 1987;14(2):167-184. PubMed | Google Scholar
- United States Centres for Disease control and Prevention (CDC). Epidemiology of meningitis caused by neisseria meningitidis, streptococcus pneumoniae, and Haemophilus influenza. Menigitis Lab manual. 2012;24(7):1-9.
- Bassey BE, Vaz RG, Gasasira AN, Braka F, Weldegriebriel G, Komakech W et al. Pattern of the meningococcal meningitis outbreak in Northern Nigeria, 200 Int J Infect Dis. 2016 Feb;43:62-67. PubMed | Google Scholar
- Kwambana-Adams BA, Asiedu-Bekoe F, Sarkodie B, Afreh OK, Kuma GK, Owusu-Okyere G et al. An outbreak of pneumococcal meningitis among older children (≥5 years) and adults after the implementation of an infant vaccination programme with the 13-valent pneumococcal conjugate vaccine in Ghana. BMC Infect Dis. 2016;16(1):1-11. PubMed | Google Scholar
- Holliman RE, Liddy H, Johnson JD, Adjei O. Epidemiology of invasive pneumococcal disease in Kumasi, Ghana. Trans R Soc Trop Med Hyg. 2007;101(4):405-413. PubMed | Google Scholar
- Moore PS. Meningococcal meningitis in sub-Saharan Africa: a model for the epidemic process. Clin Infect Dis. 1992;14(2):515-525. PubMed | Google Scholar
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID). What is meningococcal disease. NCEZID. 2020;24(7):1-5.
- Jusot J-F, Neill DR, Waters EM, Bangert M, Collins M, Bricio Moreno L et al. Airborne dust and high temperatures are risk factors for invasive bacterial disease. J Allergy Clin Immunol. 2017;139(3):977-986. PubMed | Google Scholar
- Molesworth AM, Cuevas LE, Connor SJ, Morse AP, Thomson MC. Environmental risk and meningitis epidemics in Africa. Emerg Infect Dis. 2003;9(10):1287-1293. PubMed | Google Scholar
- Ghana health services. Regional Health Directorate-Bono East. Accessed May 5, 2022.
- Ghana health services. Regional Health Directorate-Northern. Accessed May 5, 2022.
- Ghana health services. Regional Health Directorate-Upper East. Accessed May 5, 2022.
- Ghana health services. Regional Health Directorate-Upper West. Accessed May 5, 2022.
- Ghana Statistical Service. Ghana 2021 population and housing census. 2021.
- Touring Ghana. Upper West Region. 2016.
- Lingani C, Bergeron-Caron C, Stuart JM, Fernandez K, Djingarey MH, Ronveaux O et al. Meningococcal Meningitis Surveillance in the African Meningitis Belt, 2004-2013. Clin Infect Dis. 2015 Nov 15;61 Suppl 5(Suppl 5):S410-5. PubMed | Google Scholar
- Hodgson A, Smith T, Gagneux S, Adjuik M, Pluschke G, Mensah NK et al. Risk factors for meningococcal meningitis in northern Ghana. Trans R Soc Trop Med Hyg. 2001;95(5):477-480. PubMed | Google Scholar
- Hussein AS,, Shafran SD. Acute bacterial meningitis in adults; a 12-year review. Med Baltim. 2000;79(6):360-368. PubMed | Google Scholar
- Whyte D, Fitzgerald R,, Greally T. Epidemiology of bacterial meningitis (including invasive meningococcal and pneumococcal disease) in the HSE West (Clare, Limerick, Tipperary North), 1998 to 2008. 2009;25(1):1-24.
- Namani S, Koci R, Dedushi K, Raka L. Causative pathogens of bacterial meningitis in children and their susceptibility to antibiotics. 2010; 9(1):1-5.