Infant feeding practices among HIV positive mothers enrolled in selected public health institutions of Wolaita, Ethiopia: facility based multicenter cross-sectional study
Daniel Baza, Amene Abebe, Mesfin Markos
Corresponding author: Mesfin Markos Kacharo, School of Midwifery, Wolaita Sodo University, Wolaita Sodo, Ethiopia 
Received: 02 Feb 2022 - Accepted: 07 Apr 2022 - Published: 28 Apr 2022
Domain: Public Health Nursing, Global health, Maternal and child health
Keywords: Feeding practices, HIV-positive mothers, feeding options, exclusive breastfeeding, exclusive replacement feeding, HIV exposed infants, mixed feeding, pediatric HIV, recommended feeding practices
©Daniel Baza et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Daniel Baza et al. Infant feeding practices among HIV positive mothers enrolled in selected public health institutions of Wolaita, Ethiopia: facility based multicenter cross-sectional study. PAMJ-One Health. 2022;7:38. [doi: 10.11604/pamj-oh.2022.7.38.33580]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/7/38/full
Research 
Infant feeding practices among HIV positive mothers enrolled in selected public health institutions of Wolaita, Ethiopia: facility based multicenter cross-sectional study
Infant feeding practices among HIV positive mothers enrolled in selected public health institutions of Wolaita, Ethiopia: facility-based multicenter cross-sectional study
&Corresponding author
Introduction: mixed feeding practices among HIV positive mothers increases the risk of HIV transmission by 3-4 folds. Approximately 37.7 million people globally live with HIV, of these, 1.7 were children aged from 0-14 years. Globally, about 1.5 million people captured the new HIV in 2020. Nearly 90% of HIV infection among pediatrics is due to vertical transmission. However, there is no data regarding the feeding practices of HIV-positive mothers in the study area. Therefore, this study aimed to assess the magnitude of infant feeding practices among HIV-infected mothers in Wolaita, Ethiopia.
Methods: an institution-based cross-sectional study design was conducted among 146 HIV positive in selected hospitals of Wolaita from February to June 2021. A simple random sampling was employed to select health facilities. Data were collected by face-to-face interviewer who administered structured a questionnaire with document review. Data entry was done by Epi data version 3.1 and analyzed by SPSS version 25. Descriptive statistics were used to show the results.
Results: out of 146 HIV-positive mothers were involved in the study. The prevalence of exclusive breastfeeding, exclusive replacement feeding, and mixed feeding practices among mothers with HIV in the present study was found to be 49.3%, 19.9%, and 30.8% respectively in Wolaita.
Conclusion: exclusive breastfeeding and exclusive replacement feeding in the current study area was found to be significantly low when compared to global recommendations for feeding options for HIV-positive mothers. Therefore, all stakeholders are recommended to put an extraordinary effort to fill the gap.
The World Health Organization (WHO) suggests mothers with Human Immunodeficiency Virus (HIV) infection should be encouraged to give only breast milk for the first 6 months of their infant´s life [1,2]. The HIV positive mothers should commence appropriate diet after six months and continued breastfeeding at least for 12 months and may continue for 24 months while being wholly sustained for antiretroviral therapy (ART) adherence [1,3-5]. Giving breast milk is one of the foundations for child wellbeing, development, and survival strategies in areas where diarrhea, respiratory tract infections, and severe acute malnutrition are routine reasons for mortality and morbidity among infants prone to HIV [6,7]. Appropriate and exclusive breastfeeding is the essential approach for HIV-free survival of children exposed to HIV [7]. The principal way of mother-to-child transmission of HIV is during gestation, childbirth, and the postnatal period through breast milk [1,2]. Not breastfeeding of the HIV exposed infants (HEIs) in developing countries where access to clean water and safe feeding practice results in high rates of morbidity and mortality due to HIV/AIDS [8]. HIV can be transmitted to breastfeeding infants if the mother is not fully supported by ART and the risk of transmission is proportional to the period of breastfeeding. The researchers, healthcare workers, programmers, policymakers, and infected mothers are facing the challenges to reduce such transmission [7,9]. The mothers with HIV infection should not practice either mixed or exclusive replacement feeding in the first six months of age for their children if there it is not possible to access safe and sufficient formula [10,11]. Giving only the mothers´ breast milk for HEI is critical for the promotion of normal growth and development and prevention against the common childhood diseases [12,13]. Provision of both breast milk and other foods and drinks enhances the risk of HIV transmission by 3-4 folds than that of exclusive breast milk [2,4,8,14]. This is highly prevalent and urgent concern in less developed nations where access to safe and sufficient replacement feeding is limited [4,15,16].
Approximately 377 million people globally live with HIV, out of these, 1.7 were children aged from 0-14 years. Globally, about 1.5 million people captured the new HIV in 2020. Nearly 90% of HIV infection among pediatrics is due to mother-to-child transmission (MTCT) during pregnancy, delivery, and breastfeeding [7]. Approximately 70% of pediatric HIV occurs in Sub-Saharan Africa children [17]. Avoiding breastfeeding can eradicate these danger of mother-to-child HIV transmission in the post-delivery period, but mixed and not exclusive replacement feeding practices were associated with amplified infant death and illness in sub-Saharan Africa countries [7,11]. The decision on infant feeding practice in the era of HIV is a big challenge for caretakers and health care providers [7,15]. In Ethiopia, there is limited information about the feeding practices of HEIs and a few studies demonstrate that the practice is highly sub-optimal [18]. About 58% of children less than 6 months are exclusively breastfed irrespective of maternal HIV status [19,20]. Ethiopia recommends exclusive breastfeeding for 6 months and continuation of it for up to 12 months alongside complementary foods for HEIs [21]. Despite a few local studies conducted in different parts of the country; no study had been tried to assess infant feeding practices among HIV-positive mothers in the study area, Wolaita, Southern Ethiopia. Therefore, this study aimed to assess the infant feeding practices among mothers living with HIV attending PMTC and ART clinics in selected public health institutions of Wolaita, Southern Ethiopia.
Study setting, design and period: the current study was conducted in Wolaita Zone, located in Southern part of Ethiopia and 330 km from the capital city, Addis Ababa, Ethiopia (Wolaita Sodo city is the city of Wolaita). The Wolaita Zone has 16 districts and 7 city administrations. According to 2007 census statistics agency, Wolaita Zone has 5.437 million people. The Zone has one comprehensive specialized hospital, one general hospital, 8 primary hospitals, and 75 health centers, and 355 health posts. Currently Ottona comprehensive specialized, Christian general hospital, 5 primary hospitals and 6 health centers are basic providing integrated PMTC and ART services for HIV positive mothers. However, 5 healthcare facilities were selected for the current study. In all selected healthcare facilities, PMTCT service is incorporated with maternal, newborn, and child health (MNCH) including immunization services, antenatal care (ANC), post-delivery care, family planning and ART clinics. A facility-based quantitative cross-sectional study design was conducted from February to June 2021.
Population: all HIV positive mothers with children from birth-12 months of age and enrolled in public health institutions of Wolaita Zone were included in this study. HIV-positive mothers with HEIs aged from birth-12 months and who were visiting the selected public hospitals (selected healthcare facilities) for PMTCT and ART services during the data collection period were the study populations in our study.
Eligibility criteria: HIV positive mothers who were attending ART and PMTCT clinics of the selected healthcare facilities for not less than 6 months, and mothers with infants from birth to 12 months were included in the current study. Mothers living with HIV but who are too sick and not voluntary to participate in the study were excluded.
Sample size determination and sampling procedures: the appropriate sample size was determined using the sample size determination in health studies; that is using single population proportion formula [22]. The following assumptions: n = total number of mothers to be interviewed, Z = critical value at 95% confidence interval (1.96), P = infant feeding practice and associated factors among HIV positive mothers attending ART clinic in governmental health institutions of Bahir Dar Town, Amhara Regional State, Ethiopia, 2017 [8], d = marginal error between sample statistics and the population parameter (5%)
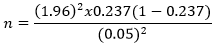
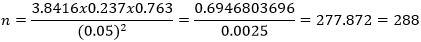
n = 288, then, 10% was added for non-response rate giving a final sample size of 311. Since the total population or the target population (the number of HIV positive mothers with HIV exposed infants which are enrolled in the selected health facilities were 231), which was less than 10, 000, the adjustment formula or reduction formula was used to get the final sample for the present study as follows:
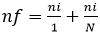
, where nf = the final sample size (146), ni = the initial sample size (311), N = the total or target population (231), nf = 311/1+311/231 = 132.547 = 133, to find the final sample size for the study, 10% of non-response rate was added making the final sample size 146.
Sampling procedures: eleven health institutions provide the integrated PMTCT services for mothers with HEIs in Wolaita. Five health facilities (Ottana comprehensive specialized hospital, Wolaita Sodo city health center, Bodit health center, Dubbo Saint Marry primary hospital, and Gassuba primary hospital) were selected by using the lottery method (simple random sampling technique) from 11 healthcare facilities with established PMTC and ART units. The study participants (HIV positive mothers) from respective health facilities with their HEIs were designated from the registration book of each health facility. The age of infants (less than 12 months during data collection period) in the selected health facilities was obtained from the record-keeping book of each healthcare facility. Probability proportion to size allocation was used to determine the appropriate sample size from the chosen healthcare facilities (Ottona teaching and referral hospital = 72, Wolaita Sodo City health center = 35, Dubbo Saint Marry primary = 18, Gassuba primary hospital = 10 and Bodit health center = 11).
Variables of the study
Dependent or outcome variable: infants feeding practice of HIV positive mothers.
Independent variables
Variables related to socio-demographic and economic characteristics of the family: age, ethnicity, religion, education of the mother, education of the husband, marital status, occupation of mother, occupation of father, economic status/monthly income, family size, exposure to mass media, place of residence, head of the family, family support.
Variables related to demographic characteristics of the infant: age and sex of the infant.
Variables related to obstetrics and health service utilization among HIV positive mothers attending PMTCT and/or ART: history and number of antenatal visits, trimester of first antenatal visit, breastfeeding counseling during antenatal visits, parity, mode of delivery, place of delivery, birth attendant, breastfeeding counseling during postnatal visits, pre-lacteal feeding, colostrum feeding, history and duration of ART usage, ARV prophylaxes for the infant and duration, time of ARV, HIV status of the infant, ART for the infant, postnatal counseling history, disclosure of HIV status.
Variables related to infant feeding practices of the HIV positive mothers: history, time and duration of breastfeeding, provision of expressed milk and the reasons, utensils used for feeding, history of exclusive replacement and mixed feeding, type of feeding given, current feeding history, time of cessation of breastfeeding and initiation of complementary feeding.
Operational definitions
Exclusive breastfeeding: providing merely mother's breast milk and no other fluids or solids, excluding the prescribed drugs and supplementations.
Recommended feeding: stopping the mixed feeding and giving only breastfeeding or only exclusive replacement feeding for the first six months after delivery.
Exclusive replacement feeding (ERF): when HIV-positive mothers stop breastfeeding and give an infant the appropriate breast milk constitutes-commercial infant formula or household created a formula with micronutrient supplements.
HIV exposed infants (HEIs): the infants born to HIV positive pregnant women are either infected or not infected (Infant born to HIV-infected mother or HIV antibody-positive infant <18 months of age.
Mixed feeding: if the other liquids and/or foods together with the breast milk given to an infant during the first six months of age.
Timely initiation of breastfeeding: starting of breastfeeding for the newborn babies immediately or within 1 hr following delivery.
Data collection tools and procedures
Tool description: the data collection tool was developed after extensively reviewing different kinds of literature published on similar topics and other relevant documents. The questionnaires were first prepared in English, translated to local Wolaitegna, and back translated to English language to check the consistence by each language expert. The developed tools were related to World Health Organization (WHO) indicators for assessing infant feeding practices among HIV positive mothers [9,23-25]. The tools were adapted to the Ethiopian context by considering the study area and its objective. The tools contained sections that assess socio-democratic characters of the respondents and infants; obstetrics related and breastfeeding practice of the mother, obstetrics and health service utilization related to practices of HIV positive mothers attending PMTCT clinics, and the prophylaxis history and HIV status of the infant. The tools were first prepared in the English language, then translated to the local language, Wolaitegna, and translated back to English by another translator to check the consistency of the data.
Data collection procedure: data were collected by a pretested, validated and structured interviewer-administered questionnaire with face-to-face interview to obtain socio-demographic and economic characteristics of the mother and document review was used to collect the other required data. Data were collected by appropriately trained four BSc nurses and four BSc midwives who are not working in the selected healthcare facilities. The medical records of study participants (HIV positive mothers-infants pair) were viewed to extract relevant information including the age of HEIs, duration of ART of the mother, WHO clinical staging of the mother, and the HIV status of the infants. Data were collected by face-to-face interview and supervision was done on the prepared checklists. The mothers' practice regarding exclusive breastfeeding practices was assessed by interviewing them whether they have provided fluids and or foods other than breast milk during the first six months of infants' age. Exclusive replacement feeding was evaluated by asking the mothers whether they fed only formula feeding. The interview was conducted during the exit period after HIV-positive mothers got services from either ART clinic or PMTCT. The interview was conducted in a place where the woman feels free to express their feelings and ideas.
Data quality management: the quality of data was assured by proper designing and pretest of the questionnaires in 5% of the sample size in health facilities with PMTCT and ART services other than the selected healthcare institutions. Five days of training were given to both data collectors and supervisors by the principal investigator on the objectives of the study, contents of the questionnaire, sampling procedures, data collection techniques, and the issues of the confidentiality of the response. The brief clarification was given to the study participants before conducting the interview, and daily based supervision of data collectors and supervisors was done by the principal investigator throughout the data collection period at each of the selected healthcare facilities. The ways of collecting the data and clarification were given on each doubt before the actual data collection. The questionnaires were reviewed and checked for completeness by the supervisors and principal investigator, and the necessary feedback was offered to the data collectors on daily bases. Any missing value and incomplete questionnaires were checked before data entry.
Data analysis and procedures: the collected data were checked for completeness and consistencies and cleaned, coded, and entered into Epi-Data version 3.02 and exported to SPSS version 25 for analysis. Any missing value was checked before the analysis of the data. Frequencies and proportions were used to summarize the variables. Finally, the results from the data were presented by using texts, tables, and figures.
Ethics approval and consent to participate: an official ethical clearance letter was obtained from Wolaita Soddo University College of Health Science and Medicine Institutional review board. Then, all the necessary communication was made with respective health administrators at selected facilities and permission letter was obtained to the officials of each facility. The respondents of the study were informed about the objectives of the study; significance of their participation, benefits, risks, and rights to withdraw any time was used. Verbal informed consent was obtained from the study participants before collecting data. The participants were assured that their involvement is voluntary and if they choose not to embrace the study, it may not affect them anyway. The respondent´s privacy and confidentiality was maintained by omitting the respondents during the data collection period.
Socio-demographic and economic characteristics of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected health facilities of Wolaita, Southern Ethiopia: a total of 146 HIV-positive mothers with children less than 12 months of age had participated in the current study making a response rate of 100%. The majority of mothers 76 (52.2%) participated in the study were in the age category of 26-34 years with the mean (+/-SD) of 7 years old. Most of the mothers in this study were married 131 (89.7%) and had attained primary education 51 (34.9). Majorities of mothers 85 (56.2%) are followers of protestant Christianity and 127 (87%) of them are Wolaita in their ethnic affiliations. The most of mothers 88 (60.3%) were housewives and 104 (71.2%) of them were urban dwellers. About 40 (27.4%) of mothers claimed their monthly income is less than 999 Ethiopian Birr. More than half 76 (52.1%) of the infants' age category was 0-6 months and 80 (54.8%) of them are males Table 1. From the total of 146 HIV-positive mothers involved in the study, 143 (97.9%) of them followed ANC and of these mothers, 97 (66.4%) attended ANC more than four times. All most of all mothers 142 (97.3%) gave birth at a health facility and the vast majorities 136 (93.2%) reported that they had a spontaneous vaginal delivery. From mothers who participated in the study, 131 (89.7%) declared that they followed postnatal care and 76 (52.1%) had been taking ART for less than 5 years. Most of the mothers 131 (89.7%) stated that they disclosed their HIV status to their spouse but about 80 (54.8%) they did not reveal their status to their close families or friends. The majority of mothers 139 (95.2%) heard about infant feeding options from healthcare workers and 140 (97.9%) of them had been counseled on infant feeding options during pregnancy 116 (79.5%), delivery 5 (3.4%), postnatal period 2 (1.4%), and ART follow-up 23 (15.8%) respectively (Table 2).
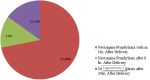
The infants' prophylaxis history in selected hospitals of Wolaita, Southern Ethiopia: among 146 HIV positive mothers who participated in the present study, 105 (71.9 %) reported that their infants had been given nevirapine prophylaxis within 1 hr after delivery, 19 (13%) subsequently following 8 hrs postnatal period and 22 (15.1%) of their infants were provided nevirapine prophylaxis after 24 hrs of post-delivery (Figure 1).
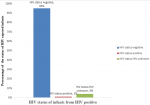
The infants' HIV status in selected hospitals of Wolaita, Southern Ethiopia: from the total of study participants, 138 (94.5%), 2 (1.4%), and 6 (4.1%) of mothers declared their infants are HIV negative, positive, and of unknown status respectively (Figure 2).
Breastfeeding practices of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected hospitals of Wolaita, Southern Ethiopia (n=146): nearly 129 (84.4) of their children were breastfed, of which approximately 108 (74.6%) of mothers practiced giving breast milk within 1 hr after childbirth. Of all HIV-positive mothers involved in the study, 72 (49.1%), 29 (19.9%), and 45 (30.8%) claimed they had been practicing exclusive breastfeeding, exclusive replacement feeding, and mixed feeding respectively during the first six months of age. The majority of mothers 113 (77.4%) reported that they continued providing breast milk for 12 months and 122 (83.6%) of study respondents initiated complementary feeding at six months of their infants-age (Figure 3).
Infant feeding practices of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected health facilities of Wolaita, Southern Ethiopia (n=146): approximately 13 (8.9%) of mothers living with HIV expressed their breast milk and 10 (6.8%) of these mothers used cups for feeding of the expressed milk. As reported from the study respondents 9 (6.1%), the main reason why they express the breast was to relieve their breast pain. None of HIV positive mothers experience feeding of heat-treated express breast milk for their HEIs (Table 3).
The current study evaluated infant feeding practices of mothers living with HIV in five selected health facilities of Wolaita, Southern Ethiopia. Infant feeding practices of HIV positive mothers in the study setting (Wolaita) is not in compliance with the WHO feeding recommendations for mothers living with HIV. Majority of the mothers, 84.4% breastfed their infants. Approximately 74.6% of the respondents who had breastfed their baby initiated breastfeeding immediately following delivery, 49.31% of mothers living with HIV infection practiced exclusive breastfeeding, 19.9% proportion of the HIV positive mothers gave exclusive replacement feeding for their HEIs, nearly 22.6% of HIV positive mothers stopped breastfeeding before their infants turned the age of 12 months. The finding from the present study had shown that majority of the mothers, 84.4% had breastfed their HEIs. This finding is in line with a study done in Kenyata University, Nairobi, Maseru, Mekele town and Shashemene which reported 91.7%, 89%, and 90.7% of HIV positive mothers had given breast milk for their newborn babies after delivery respectively [26-29]. The present study had revealed that approximately 74.6% of the respondents who had been breastfed their baby initiated breastfeeding immediately following delivery. This finding is greater than the finding of Adama and Bishoftu, Ethiopia where 70% [8] and Kenyata University, Nairobi in which 69.7% [27] of mothers initiated within 1-hour postnatal period. The differences might be due to socio-democratic and socio-cultural variations, sample size, and the facilities' health structure.
In this particular study, approximately 49.31% of mothers living with HIV infection practiced exclusive breastfeeding for their HEIs during the first six months following delivery. This result is comparatively much lower than the study report of in Northern part of Ethiopia 88.8% [30], Debre Markos Referral Hospital, East Gojam zone 85.8% [31] and Lira, Northern Uganda 77.5% [32] where of HIV positive mothers experienced only breast milk for their infants during the first six months of age. The possible explanation for variation could be due to differences in infant feeding options available, study period, sample size, level of facility, socio-economic, cultural influence, and the resources' availability as well as differences in guidelines and recommendations. The current study demonstrated that about 19.9% proportion of the respondents gave exclusive replacement feeding for their HEIs in the first six months of age. This finding is higher than the research report of Kiambu, Kenya [28], Mekele City [29], and Northern Ethiopia [30] where 3.4%, 9.3%, 4.6%, and 10.4% of HIV positive mothers provided ERF respectively but lower than the study done in Addis Ababa where 46.8% [33] proportion of mothers living with HIV used ERF. The differences might be partly due to disparities in the characteristics of study respondents, most mothers might be sticky to only a single feeding option, the inadequacy of information given for PMTCT followers, and the period of the study. This study is in agreement with different kinds of research done in various African countries.
Almost half, 45% of mothers who participated in the recent study revealed that they had been experienced mixed feeding for their HIV exposed infants during the first six months of age. This outcome is higher than the study report of Addis Ababa 15% [34], Gonder and Bahir Dar City 21.6% and 10.9% respectively [15,35,36] and is much higher than that of the study performed in South Africa and Kiambu, Kenya where only 4.3% and 18.2% [27,37] proportion of mothers with HIV infection practiced mixed feeding respectively. The likely explanation for the discrepancy in this finding might be attributable to mothers´ choice of feeding options, non-affordability or non-availability and/or inability of mothers to provide enough formula feed, lack of awareness on the danger of mixed feeding, or variability in the age of HEIs and interventional differences in health policy and programmers among the health cadres in the study area. On the other hand, the proportion of mothers who practiced mixed feeding in the present study is comparatively lower than the finding from eastern Uganda where 51% of the study respondents gave mixed feeding for their children [38]. This slight variation might be due to differences in social taboos and respondents' characteristics.
Nearly 22.6% of the mothers with HIV infection in the recent study stopped breastfeeding before their infants turned the age of 12 months. This finding is much lower than the study report in Oromia regional state where 52.6% [8] and comparatively less than the study finding of Southern part of Ethiopia 32% [39] of the study respondents ceased breast milk before 12 months for their child. Inconsistence of the study result might be due to a variety of health education delivered for the mothers during their care at healthcare facilities. This study demonstrated that nearly 16% of mothers started complementary feeding before 6 months of age for their HEIs and this is consistent with the finding similar study Southeastern part of Ethiopia where 17.5% proportion of HIV positive mothers initiated weaning practice before the age of six months for their infants.
Limitation of the study: the study is conducted among HIV-positive mothers who are attending prevention of mother-to-child transmission of HIV clinics for follow-up care. Therefore, mothers living with HIV in the community but not visiting PMTCT clinics were missed. This might be affected the generalizability of the study finding for the whole population.
The prevalence of exclusive breastfeeding and exclusive replacement feeding in the current study area was found to be 49.3%, and 19.9% respectively, which is lower than the recommended feeding options for HIV-positive mothers. The study indicates that there are poor infants feeding practices among mothers with HIV-exposed infants in the study area. Promoting HIV-positive mothers regarding appropriate infant feeding options during follow-up visits, delivering continuous health information for the mothers, may be helpful to improve the practice. The researchers also recommend there should be a strategy on infant feeding counseling that aligns to the local context and is easily understood by mothers. The mothers with HEIs should be strongly alerted to make an informed decision on the feeding options, and extraordinary effort is required to meet WHO recommended feeding practices of HIV-infected mothers in the study area.
Funding: this study did not receive any fund.
What is known about this topic
- HIV positive mothers should give only their breast milk or exclusive replacement feeding for their HIV exposed infants and avoid mixed feeding practice during the first six months of age their infants´ age. Giving breast milk is one of the foundations for child wellbeing, development, and survival strategies in areas where diarrhea, respiratory tract infections, and severe acute malnutrition are routine reasons for mortality and morbidity among infants prone to HIV;
- Provision of breast milk and other foods and/or drinks increases the risk of HIV transmission from mother to their exposed by 3-4 folds in HIV infected mothers;
- Mother living HIV infection should initiate appropriate complementary feeding at six months of age for their infants, and they should continue breastfeeding at least for 12 months of age according to World Health Organization recommendation.
What this study adds
- The prevalence of exclusive breastfeeding, exclusive replacement feeding, and mixed feeding practices among HIV positive mothers with HIV exposed infants participated in the study was found to be 49.3%, 19.9% and 30.8% respectively;
- Approximately 13 (8.9%) of mothers living with HIV expressed their breast milk and 10 (6.8%) of these mothers used cups for feeding of the expressed milk;
- None of HIV positive mothers experienced feeding of heat-treated express breast milk for their HIV exposed infants.
The authors declare no competing interests.
Daniel Baza: conceptualization, designing the study, acquisition of data, methodology, analysis and interpretation; drafting; software, writing-original draft, and writing-review & editing, revising, and critical reviewing of the manuscript. Amene Abebe: involved in methodology; analysis and interpreting the result; writing-original draft, and review and editing the manuscript. Mesfin Markos: involved in methodology; analysis and interpreting the result; writing-original draft, and review and editing the manuscript. All authors have read the final version of the manuscript and approved it possible publication.
Our heartfelt thanks also go to Wolaita Soddo University postgraduate internet resource center for their coordination or facilitation to access the respective services. We would like to thank the study respondents, focal persons working at PMTCT and ART clinics, and data collectors for their irreplaceable effort.
Table 1: socio-demographic and economic characteristics of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected health facilities of Wolaita, Southern Ethiopia, 2021 (n= 146)
Table 2: maternal service utilization history and disclosure status of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected health facilities of Wolaita, Southern Ethiopia (n=146)
Table 3: infant feeding practices of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected health facilities of Wolaita, Southern Ethiopia (n=146)
Figure 1: time of initiation of antiretroviral prophylaxis for infants following delivery in selected hospitals of Wolaita, Southern Ethiopia, 2021
Figure 2: the HIV status of infants from HIV positive mothers attending prevention of mother-to-child transmission clinics in selected hospitals of Wolaita, Southern Ethiopia, 2021
Figure 3: breast feeding practices of HIV positive mothers attending prevention of mother-to-child transmission clinics in selected hospitals of Wolaita, Southern Ethiopia, 2021
- Ciaranello AL, Leroy V, Rusibamayila A, Freedberg KA, Shapiro R, Engelsmann B et al. Individualizing the WHO HIV and infant feeding guidelines: optimal breastfeeding duration to maximize infant HIV-free survival. Aids. 2014;28 Suppl 3(3):S287-99. PubMed | Google Scholar
- WHO. Guideline: updates on HIV and infant feeding: the duration of breastfeeding, and support from health services to improve feeding practices among mothers living with HIV. 2016. Accessed Feb 2, 2022.
- WHO. HIV/AIDS. Infant feeding and nutrition. 2016. Accessed Feb 2, 2022.
- WHO guidelines approved by the guidelines review committee, in guidelines on HIV and infant feeding. Principles and recommendations for infant feeding in the context of HIV and a summary of evidence. WHO;Geneva. 2010.
- Takah NF, Atem JA, Aminde LN, Malisheni M, Murewenhema G. The impact of approaches in improving male partner involvement in the prevention of mother-to-child transmission of HIV on the uptake of safe infant feeding practices by HIV positive women in sub-Saharan Africa. A systematic review and meta-analysis. PLoS One. 2018 Dec 3;13(12):e0207060. PubMed | Google Scholar
- Chilaka VN, Konje JC. HIV in pregnancy - an update. Eur J Obstet Gynecol Reprod Biol. 2021 Jan;256:484-491. PubMed | Google Scholar
- Goon DT, Ajayi AI, Adeniyi OV. Reasons for the early introduction of complementary feeding to HIV-exposed infants in the Eastern Cape, South Africa: an exploratory qualitative study. Medicina (Kaunas). 2020 Dec 16;56(12):703. PubMed | Google Scholar
- Ejara D, Mulualem D, Gebremedhin S. Inappropriate infant feeding practices of HIV-positive mothers attending PMTCT services in Oromia regional state, Ethiopia: a cross-sectional study. Int Breastfeed J. 2018 Aug 17;13:3. PubMed | Google Scholar
- Adegbehingbe SM, Paul-Ebhohimhen V, Marais D. Development of an AFASS assessment and screening tool towards the prevention of mother-to-child HIV transmission (PMTCT) in sub-Saharan Africa-a Delphi survey. BMC Public Health. 2012 Jun 6;12:402. PubMed | Google Scholar
- Unitaid, Ukaid. HIV market report. 2019. Accessed Feb 2, 2022.
- Belay GM, Wubneh CA. Infant feeding practices of HIV positive mothers and its association with counseling and HIV disclosure status in Ethiopia: a systematic review and meta-analysis. AIDS Research and Treatment. 2019;3862098. PubMed | Google Scholar
- Lazarus R, Struthers H, Violari A. Promoting safe infant feeding practices - the importance of structural, social and contextual factors in Southern Africa. Journal of the International AIDS Society. 2013;16(1):18037-18037. PubMed | Google Scholar
- Unaids. Global HIV & AIDS statistics - fact sheet. 2021. Accessed Feb 2, 2022.
- Aidasmap N. Feeding your baby when you have HIV. 2021. Accessed Feb 2, 2022.
- Mihret MS, Asaye MM, Mengistu BA, Belete H. Mixed infant feeding practice and associated factors among HIV-positive women under care in Gondar City's Public Health Facilities within two years postpartum: a cross-sectional study. Int J Pediatr. 2020;2020:4597962. PubMed | Google Scholar
- Sethuraman K, Hammond W, Hoang MA, Dearden K, Nguyen MD, Phanet HTT et al. Challenges for safe replacement feeding among HIV-positive mothers in Hai Phong and Ho Chi Minh City, Vietnam: a qualitative study: food and nutrition technical assistance II project, in research note. Washington, DC. 2011.
- Keshmiri R, Coyte PC, Laporte A, Sheth PM, Loutfy M. Cost-effectiveness analysis of infant feeding modalities for virally suppressed mothers in Canada living with HIV. Medicine (Baltimore). 2019;98(23):e15841. PubMed | Google Scholar
- Dagnew AB, Tewabe T, Birhie A, Birehanu M, Alehegn T, Simachew A et al. Factors associated with compliance with World Health Organization-recommended infant-feeding practices by mothers with HIV infection in Northwest Ethiopia. Curr Ther Res Clin Exp. 2019 Oct 18;91:39-44. PubMed | Google Scholar
- Chaponda A, Goon DT, Hoque ME. Infant feeding practices among HIV-positive mothers at Tembisa hospital, South Africa. Afr J Prim Health Care Fam Med. 2017 Jul 27;9(1):e1-e6. PubMed | Google Scholar
- Horwood C, Haskins L, Goga A, Doherty T, John V, Engebretsen IMS et al. An educational intervention to update health workers about HIV and infant feeding. Matern Child Nutr. 2020;16(2):e12922. PubMed | Google Scholar
- Federal Minister of Health E. National guidelines for comprehensive HIV prevention, care and treatment. Addis Ababa: Minister of health, Ethiopia. 2019.
- Lwanga SK, Lemeshow S. Sample size determination in health studies: a practical manual. Geneva: World Health Organization. 1991. Google Scholar
- Aidasmap N. Feeding your baby when you have HIV. 2021.
- Ansha MG, Kuti KA, ST Tasew. Infant feeding practice and associated factors among HIV positive mothers at health institution of Shashemene Town, South Ethiopia. Journal of Family & Reproductive Health. 2020;14(2):124-130. PubMed | Google Scholar
- Health FMO. National guidelines for comprehensive hiv prevention, care and treatment. Minister of health: Addis Ababa. 2019.
- Ansha MG, Kuti KA, Tasew ST. Infant feeding practice and associated factors among HIV positive mothers at health institution of Shashemene town, South Ethiopia. J Family Reprod Health. 2020;14(2):124-130. PubMed | Google Scholar
- Andare N, Ochola S, Chege P. Determinants of infant feeding practices among mothers living with HIV attending prevention of mother to child transmission Clinic at Kiambu Level 4 hospital, Kenya: a cross-sectional study. Nutr J. 2019 Nov 2;18(1):64. PubMed | Google Scholar
- Olorunfemi SO, Dudley L. Knowledge, attitude and practice of infant feeding in the first 6 months among HIV-positive mothers at the Queen Mamohato Memorial hospital clinics, Maseru, Lesotho. Afr J Prim Health Care Fam Med. 2018 May 17;10(1):e1-e12. PubMed | Google Scholar
- Girma Y. Infant feeding practice and associated factors among HIV positive mothers enrolled in governmental health facilities in Mekelle Town, Tigray Region, North Ethiopia. Journal of HIV/AIDS and Infectious Diseases. 2013. Google Scholar
- Gejo NG, Weldearegay HG, W/Tinsaie KT, Mekango DE, Woldemichael ES, Buda AS et al. Exclusive breastfeeding and associated factors among HIV positive mothers in Northern Ethiopia. PLoS One. 2019 Jan 16;14(1):e0210782. PubMed | Google Scholar
- Wakwoya EB, Zewudie TA, Gebresilasie KZ. Infant feeding practice and associated factors among HIV positive mothers in Debre Markos Referral Hospital East Gojam zone, North West Ethiopia. Pan Afr Med J. 2016;24:300. PubMed | Google Scholar
- Napyo A, Tumwine JK, Mukunya D, Waako P, Tylleskär T, Ndeezi G. Exclusive breastfeeding among HIV exposed infants from birth to 14 weeks of life in Lira, Northern Uganda: a prospective cohort study. Glob Health Action. 2020 Dec 31;13(1):1833510. PubMed | Google Scholar
- Maru Y, Haidar J. Infant feeding practice of HIV positive mothers and its determinants in selected health institutions of Addis Ababa, Ethiopia. Ethiopian Journal of Health Development. 2010;23. Google Scholar
- Muluye D, Woldeyohannes D, Gizachew M, Tiruneh M. Infants and young children feeding practice and associated factors among HIV positive mothers of children 0-23 months in health centers of Gulele sub-city, Addis Ababa, Ethiopia. BMC Research Notes.2019;12(1):666. PubMed | Google Scholar
- Muluye D, Woldeyohannes D, Gizachew M, Tiruneh M. Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Gondar Town health institutions, Northwest Ethiopia. BMC Public Health. 2012;12(1):240. PubMed | Google Scholar
- Sendo E, Mequanint FT, Sebsibie G. Infant feeding practice and associated factors among HIV positive mothers attending ART clinic in governmental health institutions of Bahir Dar Town, Amhara Regional State, Ethiopia, 2017. Journal of AIDS & Clinical Research. 2017;09. Google Scholar
- Peltier CA, Ndayisaba GF, Lepage P, van Griensven J, Leroy V, Pharm CO et al. Breastfeeding with maternal antiretroviral therapy or formula feeding to prevent HIV postnatal mother-to-child transmission in Rwanda. Aids. 2009; 23(18):2415-23. PubMed | Google Scholar
- Fadnes LT, Engebretsen IM, Wamani H, Semiyaga NB, Tylleskär T, Tumwine JK. Infant feeding among HIV-positive mothers and the general population mothers: comparison of two cross-sectional surveys in Eastern Uganda. BMC Public Health. 2009;9:124. PubMed | Google Scholar
- Mebratu L, Mengesha S, Tegene Y, Alano A, Toma A. Exclusive breast-feeding practice and associated factors among HIV-positive mothers in governmental health facilities, Southern Ethiopia. J Nutr Metab. 2020 Sep 16;2020:7962054. PubMed | Google Scholar