One health: harmonizing infection prevention and control, and antimicrobial stewardship in combating antimicrobial resistance to improve patient safety
Mohammed Mohammed Manga, Muhammad Ibrahim Saddiq, Ahmed Aliyu Abulfathi, Yahaya Mohammed, Zainab Yunusa-Kaltungo, Adeola Fowotade
Corresponding author: Mohammed Mohammed Manga, Department of Medical Microbiology and Immunology, Gombe State University and Federal Teaching Hospital Gombe, Gombe State, Nigeria 
Received: 21 Feb 2022 - Accepted: 08 Mar 2022 - Published: 11 Mar 2022
Domain: Health system development,Laboratory medicine,Global health
Keywords: One Health, antimicrobial resistance, patient safety, antimicrobial stewardship, infection prevention and control
©Mohammed Mohammed Manga et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Mohammed Mohammed Manga et al. One health: harmonizing infection prevention and control, and antimicrobial stewardship in combating antimicrobial resistance to improve patient safety. PAMJ-One Health. 2022;7:22. [doi: 10.11604/pamj-oh.2022.7.22.33939]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/7/22/full
Perspective 
One health: harmonizing infection prevention and control, and antimicrobial stewardship in combating antimicrobial resistance to improve patient safety
One health: harmonizing infection prevention and control, and antimicrobial stewardship in combating antimicrobial resistance to improve patient safety
![]() Mohammed Mohammed Manga1,&,
Mohammed Mohammed Manga1,&, ![]() Muhammad Ibrahim Saddiq2, Ahmed Aliyu Abulfathi3,
Muhammad Ibrahim Saddiq2, Ahmed Aliyu Abulfathi3, ![]() Yahaya Mohammed4, Zainab Yunusa-Kaltungo5, Adeola Fowotade6
Yahaya Mohammed4, Zainab Yunusa-Kaltungo5, Adeola Fowotade6
&Corresponding author
One of the greatest successes in the fight against infectious diseases is the discovery of antimicrobials. This has remained a cornerstone in subsequent advancements in healthcare delivery. However, the emergence of Antimicrobial Resistance (AMR) dampened the celebrations. Currently, AMR is a major hindrance to patient safety because of the emergence, re-emergence and continued spread of multidrug resistant (MDR) pathogens. The speed and extent of AMR spread is a major threat to human health globally. Several efforts and approaches have been tried at different levels to combat this global menace. However, the continued emergence of different MDR pathogens has escalated the seriousness of the threat, especially the rising burden of healthcare associated infections. Improving antimicrobial stewardship (AMS) has been advocated worldwide to preserve the available antimicrobials for use against the right pathogens. The interrelationship between AMR, AMS, and infection prevention and control (IPC) in the context of Patient Safety can best be understood by integration into the “one health” concept. The one health concept was introduced to break barriers and minimize compartmentalization of efforts without losing the benefit of specialization and expertise in addressing human challenges. We argue that one health concept should be universally embraced and used in harmonizing all efforts at combating AMR through AMS and IPC to improve Patient Safety and healthcare quality across human, animal and environmental healthcare systems. This perspective is our effort to bring all the components under the one health umbrella.
The concept of one health, as coined by William B Karesh was based on the inter-sectoral role of different specialists in contributing to the health of humans, animals and their environment [1]. This idea came from the observation of a common link between humans, animals and their environment regarding distribution and circulation of microorganisms. No individual or specialist has all the attributes needed to overcome the multifaceted challenges facing humans. It is therefore imperative to have a holistic, multidisciplinary approach that accounts for all peculiarities and differences. This laid the foundation for the concept of one health. The concept of one health predates the current coinage and application [2]. It was similarly applied in the same context over 200 years ago initially as One Medicine [2]. Although there is no universally agreed definition across scientific/health organizations and countries, the widely circulated definition by the US Center for Disease Control and Prevention and the one health Commission is 'one health is defined as a collaborative, multisectional, and transdisciplinary approach-working at the local, regional, national, and global levels-with the goal of achieving optimal health outcomes recognizing the interconnection between people, animals, plants, and their shared environment´ [2,3]. Therefore, the one health concept provides a platform for broader understanding and an all-encompassing approach to all healthcare challenges by harnessing from knowledge shared across all disciplines of human endeavor.
Harmonizing the one health concept, with AMR, AMS, IPC and patient safety: currently, the greatest public health threat posed by microorganisms is AMR, which could be overcome by the one health concept integrating efforts at IPC and AMS to improve patient safety [4]. The rapid development and spread of AMR is a result of failure in multidisciplinary approach to AMR´s root causes and drivers as contained in the one health concept [5,6]. The United Nations Sustainable Development Cooperation Framework identified AMR as major public health threat requiring the co-operation of all member states with particular emphasis on one health as an all-inclusive concept [7,8]. The introduction of the concept of “resistome” defined as “a collection of all the antibiotic resistance genes (ARGs) and their precursors in pathogenic and non-pathogenic bacteria” further provided the needed driving force to the idea behind one health being the best umbrella to be used in studying AMR and its public health significance [9]. This provided an important guide to the understanding and conceptualization of many prevention and control measures with respect to transmission and spread of AMR in both adults and children [10].
Patient safety has been defined as “a framework of organized activities that creates cultures, processes, procedures, behaviors, technologies and environments in health care that consistently and sustainably lower risks, reduce the occurrence of avoidable harm, make errors less likely and reduce the impact of harm when it does occur.” [11]. Although the word “patient” was used, in the context of reducing healthcare associated harm, everyone can be viewed as potential patient [12]. One of the major threats to patient safety is the emergence and spread of AMR [13]. It hampers efforts of ensuring patient safety irrespective of the setting; hospital or community. Campaigns to ensure patient safety were prominent and prioritized [14]. Consequently, at the 74th World Health Assembly (WHA) in 2021, the Global Patient Safety Action Plan 2021-2030 was adopted, [11] and aimed to provide a coherent and well-articulated road map for patient safety. This is another indication of the importance the international community has attached to patient safety. One of the strategic objectives of the document was to “put in place rigorous and evidence based measures for IPC to minimize the occurrence of health care-associated infections and antimicrobial resistance” [11]. Despite the emphasis on the link between IPC and AMR in ensuring patient safety, the one health approach that provides a broader platform was virtually left out of the document. There is, therefore, the urgent need to harmonize individual components of AMR, IPC and AMS into the one health approach. This is more so that most IPC programs are linked to and also directed towards the fight against AMR [15].
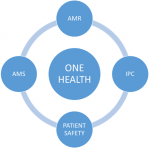
AMS efforts and strategies have been well-developed and implemented at different levels across the globe [16]. They are aimed at conserving antimicrobial by protecting them from misuse and abuse, thereby preventing the emergence of resistance [17]. Most of the AMS guidelines and strategies lack the one health approach and are mostly skewed towards human health. Compartmentalization of efforts with minimal or no central co-ordination almost two decades after the conceptualization of one health might have contributed to the inefficient fight against AMR. The misuse and abuse of antimicrobial within both hospital and community setting is pushing the development of resistance faster and similarly retarding the efforts at control/prevention. For the world to be ready for any emerging pandemic, the concept of one health must be fully developed and applied uniformly globally [18,19]. An approach that will harmonize all efforts in IPC, AMS, AMR and Patient Safety is best described using the concept of one health, which enables the participation of every human specialist without rigid demarcation (Figure 1). From environmentalists to engineers extending across to veterinarians and linking with humanities and every knowledgeable human, there is a direct or indirect role for everybody and the need for all to work together for maximum benefits [20]. Progress has been made in the development of a multidimensional matrix harmonizing knowledge and inputs from diverse fields of expertise under the platform of one health [20]. Along these lines, Dalton et al. proposed extending the concept of one health to accommodate IPC measures and AMS activities, especially in the hospital setting [21]. Multi-sectoral approach to combating AMR remains the cornerstone to any successful intervention and one health approach enhances the chances for a successful outcome [22]. This is typically obvious by virtue of the fact that AMR leads to the need for AMS which is a major requirement for effective IPC that is necessary for patient safety and all can be harmonized under one-health.
System thinking approach and the one health: although very cardinal, system thinking with optimum citizen participation in the implementation and operationalization of OH is still suboptimal [23,24]. The relatively complex interrelationships between different sectors required to achieve the OH goal must be well integrated for optimum outcomes in tackling health challenges.[23,24] Knowledge integration across all relevant disciplines is key component in the understanding and operationalization of one health [24]. Applying OH in to global health and medicine remains cornerstone to improving the quality of health system of every country that is geared towards better patient safety [25].
Recommendations the one health concept needs to be incorporated and logically applied in all efforts at combating AMR/AMS, IPC strategies and improving patient safety. At national and subnational levels, the knowledge and applicability of OH should be included in educational curricula of all relevant academic disciplines and to form part of routine continuing professional developments (CPD) of all related professions. Terms of reference (ToR) of IPC/AMS and multidisciplinary patient safety teams (MPSTs) should capture and prioritize the OH approach in all their activities. Monitoring and evaluation of healthcare quality and improvement activities should incorporate the application of OH as one of the yardsticks for optimum performance in assessments and scoring. There is need to expand the frontiers of OH knowledge in to other sciences and engineering/technological disciplines.
Although there are several evidences linking AMR, AMS, IPC, and patient safety with the concept of one health, there is little or no consideration of all under a common platform. This emphasizes the need for harmonization to improve healthcare quality and patient safety. Committees responsible for patient safety regarding AMR, AMS and IPC should have a common platform under which the one health concept can be practically utilized for maximum and long-lasting impact at all levels. More research is needed to allow evidence-informed policy decision-making on the best strategy to integrate the different activities into the one health concept.
The authors declare no competing interests.
All the authors have read and agreed to the final manuscript.
We wish to acknowledge and appreciate Prof AB Osterhaus whose symposia provided new knowledge to the authors on the concept of one health in 2017 during the annual short course for emerging leaders in medical virology at the institute of human virology, University of Maryland, United States of America.
Figure 1: an interplay between patient safety, infection prevention and control (IPC), and antimicrobial stewardship (AMS) in response to the global challenge of antimicrobial resistance (AMR) and the central role of one health in strategic improvement efforts
- William Karesh. Championing “one health”. Bull World Health Organ. 2020;98(10):652-653. Google Scholar
- Mackenzie JS, Jeggo M. The one health approach-why is it so important. Trop Med Infect Dis. 2019;4(2):88. PubMed | Google Scholar
- CDC. One health office fact sheet. 2020. Accessed October 29, 2021.
- World Health Organization. Antimicrobial resistance: a threat to global health security. 2005. Accessed October 29, 2021.
- Robinson TP, Bu DP, Carrique-Mas J, Fèvre EM, Gilbert M, Grace D et al. Antibiotic resistance is the quintessential one health issue. transactions of the royal society of Tropical Medicine and Hygiene. 2016;110(7):377. PubMed | Google Scholar
- Aslam B, Khurshid M, Arshad MI, Muzammil S, Rasool M, Yasmeen N et al. Antibiotic resistance: one health one world outlook. Front Cell Infect Microbiol. 2021 Nov 25;11:771510. PubMed | Google Scholar
- WHO. Antimicrobial resistance and the United Nations sustainable development cooperation framework: guidance for United Nations country teams. Accessed November 2, 2021.
- World Health Organization Regional Office for Europe. Antimicrobial resistance: fact sheet on sustainable development goals (SDGs): health targets. 2017. Accessed November 3, 2021.
- Kim DW, Cha CJ. Antibiotic resistome from the one-health perspective: understanding and controlling antimicrobial resistance transmission. Exp Mol Med. 2021;53(3):301-309. PubMed | Google Scholar
- Manikam L, Bou Karim Y, Boo YY, Allaham S, Marwaha R, Parikh P et al. Operationalising a one health approach to reduce the infection and antimicrobial resistance (AMR) burden in under-5 year old urban slum dwellers: the childhood Infections and pollution (CHIP) consortium. One Health. 2020;10:100144. PubMed | Google Scholar
- World Health Organization. Global patient safety action plan 2021-2030: towards eliminating avoidable harm in health care. 2021. Accessed October 29, 2021.
- Mitchell PH. Defining patient safety and quality care. In: Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses. 2008. Rockville (MD). Agency for Healthcare Research and Quality (US). PubMed | Google Scholar
- Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrobial Resistance & Infection Control. 2017;6:47. PubMed | Google Scholar
- World Health Assembly 72. Global action on patient safety. 2019. World Health Organization. Accessed October 29, 2021.
- Nicolle LE. Anti-infective drug resistance surveillance and containment team. 2001. World Health Organization. Accessed October 29, 2021
- World Health Organization. Regional Office for Europe. Antimicrobial stewardship interventions: a practical guide. 2021. Accessed November 2, 2021.
- World Health Organization. WHO policy guidance on integrated antimicrobial stewardship activities. 2021. Geneva. World Health Organization . Accessed October 29, 2021.
- Acharya KP, Subramanya SH, Neupane D. Emerging pandemics: lesson for one health approach. Vet Med Sci. 2020;7(1):273-275. PubMed | Google Scholar
- Destoumieux-Garzón D, Mavingui P, Boetsch G, Boissier J, Darriet F, Duboz P et al. The one health concept: 10 years old and a long road ahead. Frontiers in Veterinary Science. 2018;5:14. PubMed | Google Scholar
- Kahn LH. Developing a one health approach by using a multi-dimensional matrix. One Health. 2021;13:100289. PubMed | Google Scholar
- Dalton KR, Rock C, Carroll KC, Davis MF. One health in hospitals: how understanding the dynamics of people, animals, and the hospital built-environment can be used to better inform interventions for antimicrobial-resistant gram-positive infections. Antimicrobial Resistance & Infection Control. 2020;9(1):78. PubMed | Google Scholar
- World Health Organization. Multisectoral action to tackle antimicrobial resistance: thematic brief on antimicrobial resistance. 2019. Accessed October 29, 2021.
- Hitziger M, Berezowski J, Dürr S, Falzon LC, Léchenne M, Lushasi K et al. System thinking and citizen participation is still missing in one health initiatives - lessons from fifteen evaluations. Front Public Health. 2021;9:653398. PubMed | Google Scholar
- Xie T, Liu W, Anderson BD, Liu X, Gray GC. A system dynamics approach to understanding the One Health concept. PLOS ONE. 2017;12(9):e0184430.. PubMed | Google Scholar
- Machalaba C, Raufman J, Anyamba A, Berrian AM, Berthe FCJ, Gray GC et al. Applying a one health approach in global health and medicine: enhancing involvement of medical schools and global gealth centers. Annals of Global Health. 2021;87(1):30. PubMed | Google Scholar