Prevalence of intestinal parasites using formal ether concentration technique and its associated factors among school children at Dawudo primary school, Dessie, Northeast Ethiopia: a cross-sectional study
Tegenaw Tiruneh, Bekele Sharew, Haftay Hailesilassie, Tahir Eyayu
Corresponding author: Tegenaw Tiruneh, College of Health Sciences, Department Medical Laboratory Science, Debre Tabor University, Debre Tabor, Ethiopia 
Received: 20 Sep 2020 - Accepted: 05 May 2021 - Published: 17 May 2021
Domain: Bacteriology,Microbiology,Parasitology
Keywords: Intestinal parasites, infections, prevalence, school children, cross-sectional study
©Tegenaw Tiruneh et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Tegenaw Tiruneh et al. Prevalence of intestinal parasites using formal ether concentration technique and its associated factors among school children at Dawudo primary school, Dessie, Northeast Ethiopia: a cross-sectional study. PAMJ-One Health. 2021;5:7. [doi: 10.11604/pamj-oh.2021.5.7.26160]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/5/7/full
Research 
Prevalence of intestinal parasites using formal ether concentration technique and its associated factors among school children at Dawudo primary school, Dessie, Northeast Ethiopia: a cross-sectional study
Prevalence of intestinal parasites using formal ether concentration technique and its associated factors among school children at Dawudo primary school, Dessie, Northeast Ethiopia: a cross-sectional study
![]() Tegenaw Tiruneh1,&, Bekele Sharew2, Haftay Hailesilassie3, Tahir Eyayu1
Tegenaw Tiruneh1,&, Bekele Sharew2, Haftay Hailesilassie3, Tahir Eyayu1
&Corresponding author
Introduction: intestinal parasitic infections are global public health problems. It causes clinical morbidity and mortality largely in developing countries. About 25% of the world´s population are chronically infected with intestinal parasites and 1.5 to 2.7 million deaths annually. This study aimed to assess the prevalence of intestinal parasites and associated factors among Dawudo elementary school children.
Methods: a cross-sectional study was conducted at Dawudo elementary school children from March to April 2017 from 236 study participants. A systematic random sampling technique was employed to select study participants. Sociodemographic data and associated factors were collected by face-to-face interview. A stool specimen was collected and examined using both wet mount and formal ether concentration technique. Data analyses were done by using SPSS version 16 software. Binary logistic regression was done to assess the strength of association between dependent and independent variables. A p-value less than or equal to 0.05 was considered as a statistically significant association.
Results: the overall prevalence of intestinal parasite was 66.5% (95% CI: 60.4%, 72.6%). The prevalence of single, double, and triple parasites was 84.1%, 13.4%, and 2.5%, respectively. Ascaris lumbricoides were the most common 56.8%, followed by E. histolytica/dispar 9.7%. Open field defecation, untrimmed finger, and eating of uncooked vegetables were statistically significantly with intestinal parasites.
Conclusion: intestinal parasitic infections in the study area were highly prevalent and a major public health problem. Therefore, an intervention strategy that focuses on periodic deworming and health education should be designed and implemented in the area to reduce the prevalence.
Parasitic infections are caused by both intestinal helminths and protozoan parasites. About 3.5 billion of the world population, predominantly school-aged children are affected by parasitic infections. Intestinal parasitic infections are the leading causes of morbidity and mortality in low socioeconomic countries including Ethiopia. Parasitic infections are also the primary causes of iron deficiency anemia, growth retardation in children, poor school performance, physical and mental health problems in later life [1,2]. In developing countries like Ethiopia, intestinal parasitic infections often leading to high morbidity and mortality, especially where rapid population growth has not been matched by improvements in sanitation and living conditions. World Health Organization (WHO) estimates that 3.5 billion people are infected with some types of intestinal parasites. The majority of them are being children [3]. Children are particularly vulnerable group to intestinal parasitic infections because of increased contamination with soil, poor personal hygiene, incorrect selection of swimming area, contact with animals, improper waste disposal, and lack of knowledge about the prevention and control strategies [4].
School-age children carry the heaviest burden of morbidity due to intestinal parasitic infections [5]. This parasitic infection causes stunted growth, physical weakness, and poor educational achievement in school life [6]. Studies from Brazil [7], Nepal [8], and Palestine [9] have shown that the prevalence of intestinal parasitic infections among children was 58.7, 66.6, and 22.2%, respectively. The prevalence of intestinal parasitic infection among children at Kenya was 25.6% of which E. histolytica (36.7%) was more prevalent [10] and in Nigeria 22.8% of which A. lumbricoides (7.9%) was more prevalent [11].
In Ethiopia, different studies conducted in different regions depicted that the prevalence and possible associated factors are different. A study was done with Debre Elias primary schools, children, North-west Ethiopia showed a prevalence of intestinal parasite was 84.3%, of which hookworm (71.2%) was the highest burden [12]. Other studies were done in south eastern Ethiopia [13] Southeast of Lake Langano [6], Delgi school children [14], University of Gondar community school [15], and school children in Jimma zone [16], showed the prevalence of 26.2%, 27.2%, 79.8%, 34.2%, and 47.1%, respectively. Periodical assessment of intestinal parasites is very important to set future prevention and control programmers. Therefore, thus study aimed to determine the prevalence and possible associated factors of intestinal parasitic infections among school-age children.
Study design, area, and period: a cross-sectional study was conducted from March to June 2017 at Dawdo elementary school children of Dessie town, Northeast Ethiopia. The town is located 410 km away from Addis Ababa. The town has a total population of 151,174 at the time of data collection and has two Governmental hospitals, six health centers, three private hospitals, and different private and non-governmental health facilities. Among the 26 elementary schools found in the town, this school is located at the centermost spot and is thus the most accessible site for the study. In addition, children from nearby villages prefer the school as it is the most accessible one. At the time of the data collection, there were 1,052 students were present.
Sample size determination and sampling techniques: the sample size for this study was calculated by using single proportion population formula taken as 95% confidence interval (CI), 5% level of significance (Z (1-α/2) = 1.96), the prevalence of intestinal parasite infection among school children (P=77.9%) reported from other studies in Ethiopia [14] and 5% marginal error. Then the sample size was calculated as:
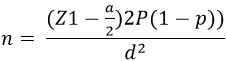
, where: n =sample size, P = prevalence of intestinal parasite infection in the study area, Z1-a/2 = CI of 95%, d = Marginal error to be tolerated. By adding 10% of contingency to minimize errors arising from the likelihood of noncompliance, 236 students were included in the study. The participating children were selected using a systematic random sampling technique by using class rosters as a sample frame. The students were stratified according to their educational levels (grade 1 to grade 8). There were 8 strata based on educational level. Then we were calculated the proportion of study participants from each stratum. The first study participants were selected randomly from each stratum. Then the next study participant was selected every Kth interval from each stratum. When the selected student was absent, the next study participant was sampled for replacement.
Socio-demographic characteristics and associated factor assessment: well-structured questionnaire based on the known associated factors was locally developed in the English version and later translated into the Amharic, the local language of the study area. The questionnaires were addressed student´s socio-demographic information and associated factors. The objectives and benefits of the study were explained to their parents. Then consents from each parent or caregiver were taken from grade one up to grade four students. Above grade five student consent was taken from each participant.
Stool sample collection and processing: after interviews, the students were clearly oriented and instructed on how to collect an appropriate and sufficient amount of sample, to avoid contamination, and bring their sample as soon as possible to the site of collection. About 2g stool specimen was collected from each student using a labeled clean, dry, wide-necked, and leak-proof plastic container. Upon arrival of the specimen, wet mount preparations were made and examined immediately. The remaining specimen was preserved using 10% formalin and transported appropriately to Wollo University Parasitology Laboratory for formolether concentration technique. The samples were processed by strictly adhering to the standard operation procedures for formolether concentration technique. The slides were examined by using 10X and 40X objectives. To increase the quality of the data about 10% of the slides (both positive and negative) were selected and reexamined by a senior parasitologist. Finally, correct recording and registration of test results were maintained.
Data analysis and interpretation: the collected data were entered into Ep-info version 7 then transferred into SPSS version 20 for analysis. Binary logistic regression analysis was used to assess the association between the dependent and independent variables. The strength of association between the associated factors and intestinal parasites was tested by odds ratio with 95% confidence intervals. In all case p-value less than 0.05 as a statistically significant association.
Socio-demographic characteristics: a total of 236 (126 males and 110 females) study participants from grade 1 to 8 were enrolled in this study. Of the total study participants majority (96.2%) were urban and the remained were rural residence. The majority of the study participants were between the age groups of 10 to 15 years (72%) (Table 1).
Prevalence of intestinal parasites: throughout the period of the current study, several species of gastrointestinal parasites (protozoa and helminths) were identified both in wet mount and formol ether concentration techniques. Out of 236 study participants, 110 (46.6%) were females from this 56 (23.7%) are infected with one or more types of intestinal parasites, 126 (53.4%) were males from this 34.3% were positive for one or more intestinal parasitic infections. Based on the finding, formol-ether concentration technique was the best method for the detection of gastrointestinal parasites, except for trophozoite stages than wet mount. The prevalence of parasitic infection was 66.5% and 36.4% by formol ether concentration technique and direct smear method, respectively (Table 2). The overall prevalence of intestinal parasite was 66.5% (95% CI: 60.4%, 72.6%). Of the total positive infected study participants, the prevalence of single, double, and triple infections was 132 (84.1%), 21 (13.4%), and 4 (2.5%), respectively (Figure 1). A. lumbricoides was the most dominant intestinal parasite (56.8%), followed by E. histolytica/dispar (9.7%), H. nana (3.4%), E. vermicularis (2.1%), H. dimuneta (1.3%), T. trichuria (1.3%), G. lamblia (0.8%), Taenia species (0.4%), S. mansoni (0.4%) and S. stercolaris (0.4%) (Table 2). Prevalence of intestinal parasite among age groups showed that 40 (25.4%), 114 (72.6%), and 3 (2%) were positives in the age group of 6 to 9, 10 to 15 and >15 years, respectively.
Associated factors of intestinal parasitic infection: among the 236 study participants, 80 (33.9%) of them used the toilet regularly of which 35 (14.8%) were positive for one or more intestinal parasites and never or sometimes use latrine was 156 (66.1%) among those 122 (51.7%) were positive. Among the potential associated factors explored using logistic regression analysis unable to use of the latrine (open field defecation), unable to wash hands before eating, untrimmed fingernail, and habit of eating uncooked vegetables were statistically significantly associated with the prevalence of intestinal parasitic infections (P< 0.05). However, the Source of water, shoe-wearing habit, and eating of raw meat were not statistically significant associations with intestinal parasitic infections (p > 0.05 (Table 3).
The present study tries to figure out the prevalence of intestinal parasites among schoolchildren. The overall prevalence of intestinal parasites was 66.5%. On the other hand, the prevalence of single, double, and triple parasites was 84.1%, 13.4%, and 2.5%, respectively. There were different kinds of literature conducted that supports our finding (66.5%) like in Dona Berber primary school, Bahir Dar (65.5%) [17], in Motta Town, Western Amhara, Ethiopia (68.4%) [18], in Atse fasil general elementary school, Azezo, Ethiopia (72.9%) [19], in Sasiga District, Southwest Ethiopia (62.4%) [20], in rural and urban school-aged children in Nigeria 67.4% [21], Jimma town (66.7%), and Nepal 66.6% reported [8]. On the contrary, the current study prevalence of intestinal parasites was lower than previously reported results from different regions of Ethiopia such as in Dagi primary school (77.9%) [22], in Delgi, North Gondar 79.8% [14], in Chencha town, Southern Ethiopia 81.0% [23], Southeast Ethiopia close to Lake Langano 83.8% [6] and Debre Elias primary schools East Gojjam Zone, Ethiopia (84.3%) [12]. The low rate of detection of intestinal parasites observed in this study may be due to differences in the method of sample collection, isolation and identification of differences in climatic conditions, environmental sanitation, economic and educational status of the study subjects, and previous control efforts in these different areas.
On the other hand, the prevalence of intestinal parasites in the current study was higher than studies reported from Gondar (34.2%) [15], Jimma, Ethiopia (47.1%) [16], in Arba Minch town, Southern Ethiopia (27.7%) [24], in Debre Birhan, Ethiopia (17.4%) [25], in Medebay Zana wereda, North Western Tigray, Ethiopia (12.7%) [26], in Shashamane town, southern Ethiopia (19.7%) [27] in Benishangul-Gumuz Regional State, Western Ethiopia (35.44%) [28]. This high prevalence could be due to the living and the socioeconomic nature of the study subjects or may be associated with the local endemicity of the parasite and geographic condition of the study area. The other possible reason for the difference might be due to differences in awareness of the people on personal and environmental hygiene from the continuous health education made by the different health educators in the different health institutions against intestinal parasites.
Our findings showed that A. lumbricoides (56.8%) (Table 2) was the predominant species which were higher than the finding reported in Ethiopia, around lake Langano (6.2%) [6], University of Gondar community school (5.9%) [15], Jimma zone (14.7%) [16], Babile (3.9%) [29], Delgi school children (48%) [14], in Dona Berber primary school, Bahir Dar (13.6%) [17]. This might be due to the problem related to environmental sanitation and personal hygiene of study subjects probably play an important role for the higher prevalence rate of Ascariasis. The present study also assessed the possible associated factors of intestinal parasitic infection. Based on our findings, children who did not use toilet (open field defecation) were likely to increase the odds of intestinal parasitic prevalence by 28.3% times (95% CI: 3.63, 220.2) than used the toilet regularly. Children who did not trim their fingernail was more likely to increased intestinal parasitic infection with the odds of 3.06 (95% CI: 1.69-5.56) than trimmed fingernail status. Handwashing habits before eating (odds ratio: 3.12, 95% CI: 1.71, 5.7), and habit of eating raw vegetables (odds ratio: 2.62, 95% CI: 1.01, 6.79) were statistically significantly associated with intestinal parasitic infections. These were in line with the study conducted in Delgi [14], Dagi primary school children [22], in Azezo, District, southwest Ethiopia, Benishangul-Gumuz Regional State, and Shashamane town [19,20,27,28]. This might be probably due to the related growing of vegetables in faecally polluted gardens, personal and environmental sanitation problems, and low knowledge of children about the transmission, prevention, and control strategies of intestinal parasitic infections.
The current study found that the magnitude of the intestinal parasite was very high health problems among the study area, which needs great effort to reduce this prevalence. The high prevalence of intestinal parasites is also associated with improper use of latrine, poor handwashing habits before eating and after defecation, untrimmed finger, and the habit of eating uncooked vegetables. In conclusion, avoiding consumption of uncooked vegetables, properly trimming their finger, proper washing of their hand before eating, and regular use of toilets may be decreasing the magnitude of the problems. In addition to this, early intervention strategies like deworming should be designed and implemented by governmental organizations. Similarly, the health care provider should be giving programmed health education and awareness creation about the transmissions, prevention, and control strategies of intestinal parasitic infection within the community.
What is known about this topic
- The finding showed a high prevalence of intestinal parasites among the study area;
- The most dominant intestinal parasite was Ascaris lumbricoides;
- Personnel and environmental hygiene are very important to reduce the prevalence of intestinal parasites.
What this study adds
- This study adds formol ether concentration techniques is better than direct or wet mount techniques to detect ova/egg of the parasites;
- Better sensitive technique to detect low parasites in a given sample.
The authors declare no competing interests.
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Tegenaw Tiruneh, Tahir Eyayu, Bekele Sharew, and Haftay Hailessilassie. The first draft of the manuscript was written by Tegenaw Tiruneh and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
The authors like to thank Wollo university, college of medicine and health sciences department of medical laboratory Sciences for providing materials and reagents to examine the stool samples. Then warmest gratitude also goes to the Director and teachers of Dawudo elementary school for their participation, assistance and cooperation in doing this research. They are also indebted to the study participants and data collector.
Table 1: socio-demographic characteristics of children among Dawudo elementary school, Dessie town, Northeast Ethiopia, March to June 2017
Table 2: comparison of wet mount and formol ether concentration technique for detection of different intestinal parasites among Dawudo elementary school children, Dessie, Ethiopia, 2017
Table 3: associated factors of IP infections among Dawudo elementary school students, Dessie, Northeast Ethiopia, March to June, 2017
Figure 1: the prevalence of single, double, and triple intestinal parasites among Dawudo elementary school, Dessie, Northeast Ethiopia
- WHO. Intestinal parasite: burden and trends. 2013.
- WHO. Prevention and control of schistosomiasis and soil-transmitted helminthiasis: report of a WHO expert committee. 2002. Google Scholar
- WHO. Training manual on diagnosis of intestinal parasites: tutor's guide (electronic resource). Geneva: World Health Organization. 2004.
- Adedayo O, Nasiiro R. Intestinal parasitoses. Journal of the National Medical Association. 2004;96(1):93. PubMed | Google Scholar
- Nies MA, McEwen M. Community/public health nursing-e-book: promoting the health of populations. Elsevier Health Sciences. 2014.
- Legesse M, Erko B. Prevalence of intestinal parasites among schoolchildren in a rural area close to the southeast of Lake Langano, Ethiopia. The Ethiopian Journal of Health Development (EJHD). 2004;18(2). Google Scholar
- Maia MMM, Fausto MA, Vieira ELM, Benetton MLFN, Carneiro M. Intestinal parasitic infection and associated associated factors, among children presenting at outpatient clinics in Manaus, Amazonas state, Brazil. Annals of Tropical Medicine and Parasitology. 2009;103(7):583-591. PubMed | Google Scholar
- Sharma BK, Rai SK, Rai DR, Choudhury DR. Prevalence of intestinal parasitic infestation in school children in the northeastern part of Kathmandu Valley, Nepal. Age. 2004 Sep;35(3):501-5. PubMed | Google Scholar
- Hussein AS. Prevalence of intestinal parasites among school children in northern districts of West Bank? Palestine. Tropical Medicine & International Health. 2011;16(2):240-244. PubMed | Google Scholar
- Mbae CK, Nokes DJ, Mulinge E, Nyambura J, Waruru A, Kariuki S. Intestinal parasitic infections in children presenting with diarrhoea in outpatient and inpatient settings in an informal settlement of Nairobi, Kenya. BMC infectious diseases. 2013;13:243. PubMed | Google Scholar
- Agbajelola V. Prevalence of intestinal helminths and protozoa parasites of ruminants in Minna, North Central, Nigeria. IOSR Journal of Agriculture and Veterinary Science. 2015;8(11):62-67. Google Scholar
- Workneh TA Esmael, Ayichiluhm M. Prevalence of intestinal parasitic infections and associated factors among Debre Elias primary schools children, East Gojjam Zone, Amhara region, North West Ethiopia. J Bacteriol Parasitol. 2014;5(1):1. PubMed | Google Scholar
- Tulu BS Taye, Amsalu E. Prevalence and its associated risk factors of intestinal parasitic infections among Yadot primary school children of South Eastern Ethiopia: a cross-sectional study. BMC research notes. 2014;7(1):848. Google Scholar
- Ayalew AT Debebe, Worku A. Prevalence and risk factors of intestinal parasites among Delgi school children, North Gondar, Ethiopia. J Parasitol Vector Biol. 2011;3(5):75-81.
- Gelaw A, Anagaw B, Nigussie B, Silesh B, Yirga A, Alem M et al. Prevalence of intestinal parasitic infections and risk factors among schoolchildren at the University of Gondar Community School, Northwest Ethiopia: a cross-sectional study. BMC public health. 2013;13:304. PubMed | Google Scholar
- Yami A, Mamo Y, Kebede S. Prevalence and predictors of intestinal helminthiasis among school children in Jimma zone; a cross-sectional study. Ethiopian Journal of Health Sciences. 2011;21(3). PubMed | Google Scholar
- Hailegebriel T. Prevalence of intestinal parasitic infections and associated risk factors among students at Dona Berber primary school, Bahir Dar, Ethiopia. BMC Infectious Diseases. 2017;17(1):362. PubMed | Google Scholar
- Asemahagn MA. Parasitic infection and associated factors among the primary school children in Motta town, western Amhara, Ethiopia. Am J Pub Health. 2014;2(6);248-54. Google Scholar
- Mengistu Endris, Wossenseged Lemma, Yeshambel Belyhun, Beyene Moges, Aschalew Gelaw, Belay Anagaw et al. Prevalence of intestinal parasites and associated risk factors among students of Atse Fasil general elementary school Azezo, Northwestern Ethiopia. Ethiop J Health Biomed Sci. 2010;3(1):25-33. Google Scholar
- Sitotaw B, Shiferaw W. Prevalence of intestinal parasitic infections and associated risk factors among the first-cycle primary Schoolchildren in Sasiga District, Southwest Ethiopia. Journal of Parasitology Research. 2020 Mar 13;2020:8681247. PubMed | Google Scholar
- Opara KN, Udoidung NI, Opara DC, Okon OE, Edosomwan EU, Udoh AJ. The impact of intestinal parasitic infections on the nutritional status of rural and urban school-aged children in Nigeria. International Journal of MCH and AIDS. 2012;1(1):73-82. PubMed | Google Scholar
- Alamir M, Awoke W, Feleke A. Intestinal parasites infection and associated factors among school children in Dagi primary school, Amhara National Regional State, Ethiopia. Health. 2013;5(10);5 Google Scholar
- Abossie A, Seid M. Assessment of the prevalence of intestinal parasitosis and associated risk factors among primary school children in Chencha town, Southern Ethiopia. BMC Public Health. 2014;14:166. PubMed | Google Scholar
- Haftu D, Deyessa N, Agedew E. Prevalence and determinant factors of intestinal parasites among school children in Arba Minch town, Southern Ethiopia. Am J Health Res. 2014;2(5):247-4. Google Scholar
- Zemene T, Shiferaw MB. Prevalence of intestinal parasitic infections in children under the age of 5 years attending the Debre Birhan referral hospital, North Shoa, Ethiopia. BMC research notes. 2018;11(1):58. PubMed | Google Scholar
- Teshale T, Belay S, Tadesse D, Awala A, Teklay G. Prevalence of intestinal helminths and associated factors among school children of Medebay Zana wereda; North Western Tigray, Ethiopia 2017. BMC Research Notes.2018;11(1):444. PubMed | Google Scholar
- Biniyam Sahiledengle, Sharbuddin Beker, Yilikal Girum, Gemeda Haji, Seid Merewo, Worksew Anberbir. Prevalence and risk factors of intestinal parasites among primary school children in Shashamane town, southern Ethiopia. MOJ Public Health. 2020;9(3):55-61. Google Scholar
- Gebretsadik G. Prevalence of intestinal parasites and associated risk factors among schoolchildren of Homesha district (Woreda) in Benishangul-Gumuz regional state, western Ethiopia. J Fam Med Health Care. 2016;2(4):57-64. Google Scholar
- Tefera E, Mohammed J, Mitiku H. Intestinal helminthic infections among elementary students of Babile town, eastern Ethiopia. Pan African Medical Journal. 2015 Jan 20;20:50. PubMed | Google Scholar