Breastfeeding practice and associated factors among mothers of children aged 6-12 months southern Ethiopia, 2023: a community-based cross-sectional study
Mahlet Birhane Estifanos, Ansha Seid Abegaz, Selamawit Semagn Kebede, Mihret Tesfu Legese, Gizaw Sisay, Hiwot Hailu Amare
Corresponding author: Mahlet Birhane Estifanos, Department of Human Nutrition, College of Health Science and Medicine, Dilla University, Dilla Ethiopia 
Received: 15 Nov 2023 - Accepted: 16 Jan 2024 - Published: 19 Jan 2024
Domain: Child nutrition
Keywords: Infant, breastfeeding practice, Gedeo zone, Ethiopia
©Mahlet Birhane Estifanos et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Mahlet Birhane Estifanos et al. Breastfeeding practice and associated factors among mothers of children aged 6-12 months southern Ethiopia, 2023: a community-based cross-sectional study. PAMJ-One Health. 2024;13:3. [doi: 10.11604/pamj-oh.2024.13.3.42182]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/13/3/full
Research 
Breastfeeding practice and associated factors among mothers of children aged 6-12 months southern Ethiopia, 2023: a community-based cross-sectional study
Breastfeeding practice and associated factors among mothers of children aged 6-12 months southern Ethiopia, 2023: a community-based cross-sectional study
![]() Mahlet Birhane Estifanos1,&, Ansha Seid Abegaz2, Selamawit semagn Kebede2, Mihret Tesfu Legese3,
Mahlet Birhane Estifanos1,&, Ansha Seid Abegaz2, Selamawit semagn Kebede2, Mihret Tesfu Legese3, ![]() Gizaw Sisay3, Hiwot Hailu Amare3
Gizaw Sisay3, Hiwot Hailu Amare3
&Corresponding author
Introduction: one of the highest infant mortality rates in the world is found in Ethiopia and improper infant feeding is a major contributing factor. Therefore, this study aimed to assess breastfeeding practice and associated factors among mothers of children aged 6 to 12 months in southern Ethiopia.
Methods: a community-based cross-sectional study of 623 participants was used. A multistage sampling technique was used and participant selection was done using proportional allocation. Data was entered into epi data version 3 and SPSS version 24 was used for cleaning and analysis. The effects of explanatory variables on the dependent variable were estimated using bivariate and multivariate logistic regression models. Results were presented with adjusted odds ratios with a 95% confidence interval.
Results: the prevalence of sub-optimal breastfeeding practice in this study is 60.2(95%CI 56.3-64). The mean (± SD) age of the index child was (8.8 ± 1.85) months. The majority (70.9%) of newborns lived in rural areas and about half (53.9%) were female. Knowledge [AOR: 0.23; 95%CI 0.15-0.35], attitude, [AOR: 2.43; 95%CI 1.14-5.21], Caesarean section delivery [AOR: 3.89; 95%CI 2.33-6.49], paternal education [AOR: 2.23; 95%CI 1.08-4.62] and breastfeeding counseling [AOR: 2.04; 95%CI 1.21-3.39] had significantly associated with the outcome variable.
Conclusion: more than half of the study participants practiced sub-optimal breastfeeding. Paternal education, knowledge, attitude, breastfeeding counseling and caesarean section (C/S) delivery. Integrating breastfeeding promotion education into routine antenatal care follow-up and strong community-based behavior change communication is recommended.
Breastfeeding is a type of food that is accessible to children everywhere and does not differentiate depending on socioeconomic class [1-3]. Adopting the best newborn and young child feeding practice throughout the two years is essential for promoting health, optimal growth, behavioral development, and cognitive performance [4]. A 13% annual fatality rate for children under the age of five is caused by inadequate breastfeeding [5]. After six months of just breastfeeding, the United Kingdom (UK) saw a 53% drop in hospital admissions for diarrhea and a 27% drop in respiratory tract infections [6]. Additionally, it has been determined that not breastfeeding results in annual economic losses of around $302 billion, or 0.49 percent of the world's gross national Gross Domestic Product (GDP) [7]. Millions of people die each year from inadequate feeding, which is responsible for 10% of all diseases worldwide [8]. Breastfeeding consistently ranks higher than having access to water and sanitary facilities as a risk factor for children's health in all developing countries [9].
According to estimates, the finest nursing practices may save 1.5 million children each year. But of the 129 million children born each year, just a small proportion receive proper nursing, and some do not receive any at all [10]. Compared to improved breastfeeding practices, unimproved breastfeeding practices considerably raise the risk of all-cause mortality [11]. According to estimates, infants under six months who are not exclusively breastfed have a more than five-fold increased risk of morbidity and mortality from pneumonia and diarrhea [12]. Infants who are breastfed have a minimum six-fold higher likelihood of surviving the first few months than infants who are not nursed [13]. According to findings from secondary data, infants who are mostly, somewhat, or not breastfed have higher chances of dying from any cause than babies who are breastfed [14].
Recent studies show that suboptimal breastfeeding practices cause 11.6% of deaths in children under the age of five. According to a 2010-2018 survey of 57 low- and middle-income nations, lower-middle-income countries had a lower prevalence (58.2%) of the introduction of solid, semi-solid, or soft food at 6-8 months, than high-income countries (81.7%) [15]. According to this study's finding, the World Health Organization (WHO) target for breastfeeding prevalence in low- and middle-income countries is still not being met [16]. Poor breastfeeding practice contributes to the deaths of 1.4 million people and 10% of the illness burden among children under the age of five [13]. Nevertheless, the public at large, healthcare professionals, and governments have given little attention to this straightforward preventive measure.
Inappropriate feeding practices are a major contributing factor to Ethiopia's newborn death rate. According to a community-based cross-sectional study, only 14.4% of mothers in the Sidama region practice optimal breastfeeding, which contributes to stunting [17]. Nearly all (97%) of children in Ethiopia have nursed at some point, making breastfeeding a widespread practice. However, a large percentage of women do not use it to its full potential [18]. Community health extension personnel and other healthcare professionals have provided various interventions, such as breastfeeding promotion, in health institutions and at the community level. Although there has already been research on breastfeeding, it solely looked at the specific breastfeeding markers [19]. Therefore, the purpose of this study is to identify suboptimal breastfeeding practice and its associated factors among mothers of children aged 6 to 12 months in Gedeo Zone southern Ethiopia by using a composite measure.
Study area and study period: the study was carried out in Gedeo Zone, which is in South Nation Nationality and People Regional State (SNNPRS), 90 kilometers from Hawassa, the region's capital city, and 369 kilometers from Addis Ababa to the Southern Addis Ababa-Moyale International route. The land area of the area is estimated to be 1347.04 square kilometers. Geographically, the zone is situated between 50 53'N and 60 27'N Latitude and between 380 8' and 380 30' East, Longitude, North of the Equator. The elevation varies from 1500 to 3000 meters. With an area of 1,210.89 square kilometers, it has eight districts, two city administrations, and a total population of 1,086,768 (49%) men and (51%) women). There are 164 kebeles in the zone, including 31 urban and 133 rural kebele. There are 276 health facilities altogether in the area, including one general hospital, three district hospitals, 38 health centers, 146 health posts, 5 Non-Governmental Organizations (NGO)´s clinics, 36 private clinics, and 47 drug vendors [20]. Community based cross-sectional study was employed from February 30 to March 30 of 2023.
Source population, study population and eligibility criteria: mothers of all infants in the Gedeo zone were the source population, while mothers of infants aged 6 to 12 months living in the selected kebele were the study population. Mothers who had lived in the selected kebele for at least 6 months were included in the study.
Sample size determination and sampling procedure: sample size was calculated by using the technique to estimate a single population proportion formula using the following assumptions.
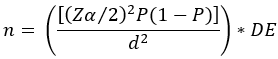
Where n= required sample size; Zα/2 = critical value for normal distribution at 95% confidence interval which equals to 1.96 (Z value at alpha=0.05); P= prevalence of sub-optimal breastfeeding practice (56.9%) among mothers who have 6-12 months of age children in Hula district, sidama zone, Ethiopia [21]; d= an absolute precision; and D=design effect.
Assumptions: with the assumptions of 95% confidence interval, 5% desired precision, prevalence 56.9 % , and design effect (D=1.5) was applied. The formula yields n=566. For 2nd specific objective, the sample size was calculated by using epi info version7 based on minimum detectable OR, 5% level of significance, and power 80%, 95% CI (Table 1). The largest sample size was the one which is calculated for the first specific objective which is 566 and adding 10% non-response rate it becomes 623.
Sampling procedure: Gedeo zone was stratified into districts (rural) and city administrative using a multi-stage sampling technique. Two districts Wonago and Dilla Zuria were chosen at random from the eight districts in the Gedeo zone. Dilla town was chosen randomly among the two cities administrative. From nine kebeles of Dilla town, the three kebeles (Buno, wooden and boete) were randomly selected. From 21 kebeles of Wonago woreda, 6 kebeles (Mokonisa, Dodora, jemjemo, tutufela, tokicha and hasse) and from15 kebele of Dilla zuria woreda, 5 kebeles (chichu, sisota, tumticha, andida, and Udo) were randomly selected. By conducting a census, houses with infants aged 6 to 12 months at each study kebele were identified. During the study period, there were 1880 infants in the chosen kebele who were between the ages of 6 and 12 months. Then the total sample was proportionally allocated to each kebele according to the number of 6 to 12-month-old infants. Using a sampling frame created from the census, households from each designated kebele were chosen using a systematic random sampling technique. Before commencing, lists of houses were created, and one was chosen at random to serve as the starting house. The next step is selecting homes at predetermined intervals or every third home (1880/623 = 3). In a household with more than one eligible study participant; one of them was chosen at random to participate in the study.
Data collection instrument: nine breastfeeding knowledge questions that were created based on the recommendations of the Infant and Young Child Feeding (IYCF) group were used to gauge participants' knowledge of breastfeeding [22]. Based on the number of questions in the knowledge segment that were correctly answered, a knowledge score was determined for each participant. Each appropriate response received a point [1] and an incorrect response scored [0]. The mean value was used to classify respondents' knowledge levels as either good or poor. This led to the values above or equal to the mean are considered to have good knowledge, whereas values below the mean are considered to have weak knowledge. Nine questions on a five-point Likert scale, from strong disapproval to high approval, were used to assess women's views towards nursing [23]. The range of answers to the attitude questionnaire was 0 to 36. The range of answers to the attitude questionnaire is 0 to 36. The mean value was used to classify respondents' attitudes towards breastfeeding as either good or poor. Respondents with scores below the mean were classified as having a negative attitude, while those with scores equal to or above the mean were classified as having a positive attitude.
The eight core yes/no feeding practices-early initiation of breastfeeding (within one hour of delivery), colostrum feeding, on-demand feeding, exclusive breastfeeding, pre-lacteal feeding, mother eating at least one additional meal, beginning complementary feeding by the age of six and breastfeeding has been sustained for at least a year (present situation) were used to construct the best breastfeeding practice [23]. All improper nursing behaviors received a score of 0, whilst all advised breastfeeding behaviors received a score of 1. The scores of each practice included in the index construction were then added up to provide a possible range of 0 to 8, and the combined score was separated into three groups. Summation scores of 0-3 were considered poor, 4-6 were considered medium, and 7-8 were considered high. Infants with high BPI scores were deemed to have received optimal breastfeeding, whereas infants with low and medium BPI scores were deemed to have received suboptimal breastfeeding [19].
Definition of terms
Optimal breastfeeding: mothers who achieve the highest tertiles on the global recommendations for breastfeeding practices are classified as practicing optimal breastfeeding mothers.
Sub-optimal breastfeeding: those mothers who achieve the lowest two tertiles are considered practicing sub-optimal breastfeeding [23].
Good knowledge: participants were divided into two groups based on their responses to the nine closed-ended questions regarding the ideal breastfeeding recommendation: those who scored mean and above the mean value were regarded to have good knowledge.
Poor knowledge: those mothers who scored below the mean value were leveled to have poor knowledge.
Positive attitude: those mothers who scored at or above the mean were categorized as having a positive attitude.
Negative attitude: participants who scored below the mean were categorized as having a negative attitude.
Data collection procedure: pre-tested structured interviewer-administered questions were developed from different literature [18]. A house-to-house visit was utilized to gather the data, and a household was employed as the sampling unit. To avoid any overlap or double counting, the first residence was chosen at random and marked with a marker. If there are two or more eligible newborns, one was chosen at random. To reduce the non-response rate as much as possible, visits were made three times if a respondent was not present. The questionnaire was first produced in English and was translated into Amharic. A 10th-grade complete data collector and supervisors with better experience in data collection were recruited.
Data processing and analysis: following the completion of the data collection procedures, the collected data was coded, put into Epi-data version 3.1, and then exported to SPSS version 20 for cleaning and analysis. Concerning socio-demographic and other independent variables, the study population was described using frequencies, means, standard deviations, and percentages. The effects of explanatory variables on the dependent variable were estimated using bivariate and multivariable logistic regression models; variables with a P-value of less than 0.2 were taken into account in the multivariate logistic analysis.
Data quality control: three-day training for data collectors and supervisors was given. A pretest was also done among five percent (31) of the study subjects. The thoroughness and cleanliness of the data were always carried out under the direct supervision of the supervisor and lead investigator. A supervisor and the primary investigator regularly examined the obtained data for accuracy, completeness, clarity, and consistency.
Ethical considerations: Dilla University Institutional Review Board granted ethical approval. The study objectives were communicated to the study subjects at the time of data collection, and their verbal and written consent was obtained to determine whether they were willing to participate or not. All the methods explained in this study were performed per the relevant guidelines and regulations.
Socio-demographic characteristics of study participants: a total of 623 mothers planned to participate; all of them have participated in this research making a response rate of 100%. The mean age and standard deviation (± SD) of the respondent was (29 ± 5.83) years. More than half (62.3%) of infants were between the ages of 6 and 9 months. The mean age and standard deviation (± SD) of the index child was (8.8 ± 1.85) months. In this study, the majority of newborns (70.9%) lived in rural areas and more than half (53.9%) of them were female. The majority (92.8%) of the respondents surveyed reported that they were married at the time of the study. The husband led the majority of households (80.7%). Only 11.7% of the mothers had a college degree or higher education. Additionally, 32.3 % of fathers had a secondary education, while 27% had a college degree or higher. One child under the age of five lived in the households in fifty percent (50.2%) of the respondents. More than half of the households (64.5%) have five or more members in their family (Table 2).
Socio economic characteristics of study participants: the study revealed that more than half of the mothers (63.3%) were housewives, while 52.3% of fathers worked as farmers. Thirty-four (34%) of study participants came from households with a monthly income of less than 9 USD (Table 3).
Obstetric and service-related factors of respondents: in the current study, the majority (87%) of mothers had received antenatal care (ANC), of these, more than half (62.4%) had 1-3 ANC follow-ups, 64.4% of study participants had postnatal follow-ups, 87.2% of participants were using family planning, the majority (75.8%) of mothers gave birth in health facilities, and 76.6% of mothers were assisted by medical personnel. The majority of moms (79.3%) gave birth vaginally, and 56.2% had two or more live deliveries. About 78% of the pregnancies were planned. More than half, 66.6% of mothers had received breastfeeding counseling (Table 4).
Knowledge related characteristics of respondents: in terms of maternal awareness, nearly a third (34%) of research participants were aware that formula milk or gruel can be used in place of breast milk. The majority of moms (74.6%) were unaware of the advantages of colostrum for the newborn. The majority of mothers, 90.4% were aware that the infants should be breastfed frequently (8-12 times per day). More than half of the participants, 63.6%, lack enough understanding of the best practices of breastfeeding (Table 5).
Attitude related characteristics of respondents: about half 50.6% of the mothers believed that the initiation of breastfeeding within one hour of birth is important. Over a third 46.7% of mothers believed that feeding colostrum (first milk) during the first days of births is important. Forty-four percent (44%) of mothers believed that at least one additional meal throughout lactation is needed for lactating mothers. Overall, 83.8% of mothers had a positive attitude toward optimal breastfeeding practice (Table 6).
Prevalence of sub-optimal breastfeeding practice: in the current study, sub-optimal breastfeeding practice among mothers was 60.2% (95% CI 56.3-64). Mothers who did not start breastfeeding right away after giving birth were 11.7%. About half (51.5%) and 43% of the mothers have not practiced breastfeeding exclusively and introduced complementary food before the baby was six months old respectively. The majority (89.2%) of moms have provided pre-lacteal meals. The most common (47%) and least common (36.6%) pre-lacteal foods provided to newborns were Amessa (local cultural medicine made from “tenaadam” and other roots) and cow's and (formula) milk, respectively. A third (32.4%) of women has thrown away colostrum (first milk) because they thought it was not clean.
Factors associated with sub-optimal breastfeeding practice: eighteen variables were potential candidates (P < 0.25) for multivariable logistic regression, including education of the mother and father, marital status, pregnancy intention, ANC presence and number, breastfeeding counseling during ANC, knowledge, attitude, and place and mode of delivery, delivery assistant, place of residence, number of under-five children in the household, maternal occupation, child's age, family monthly income, and family size.
Five variables like knowledge, attitude, mode of delivery, father education, and breastfeeding counseling during ANC retained their significant association when confounding variable effects were taken into account in the multivariate logistic regression analysis. This study discovered the association between birth methods and inadequate feeding. Contrary to individuals who gave birth via Spontaneous Vaginal Delivery (SVD), study participants who gave birth through Cesarean section were 3.89 times more likely to provide their children with suboptimal breastfeeding [AOR: 3.89; 95% CI (2.33-6.49)].
Sub-optimal breastfeeding practice was also associated with the knowledge and attitude of study participants. Study participants who had a high understanding of breastfeeding practice were 77% less likely to have sub-optimal breastfeeding practice than their counterparts [AOR: 0.23; 95% CI (0.15-0.35)]. Additionally, there is a strong association between attitude and breastfeeding practice. Participants in the study who have negative attitudes about breastfeeding practices were 2.43 times more likely than their counterparts to practice breastfeeding sub-optimally [AOR: 2.43; 95% CI (1.14-5.21)]. Similarly to this, counseling regarding breastfeeding during ANC was strongly linked to sub-optimal breastfeeding practice. In accordance with this, study participants who did not receive breastfeeding counseling during ANC were 2.04 times more likely to practice it inadequately than their counterparts [AOR: 2.04; 95% CI (1.21-3.39)].
Finally, this study discovered that breastfeeding practice was significantly predicted by the education of the father. Accordingly, respondents without parental education had 2.23 times more likely to practice inadequate breastfeeding than fathers with only secondary education [AOR: 2.23; 95% CI (1.08-4.62)] (Table 7).
The purpose of this study was to determine the prevalence of inadequate breastfeeding practice and related factors in the Gedeo zone, southern Ethiopia. The investigated area had a prevalence of sub-optimal breastfeeding practice of 60.2% (95% CI: 56.3 - 64.0). Educations of the father, respondent knowledge, breastfeeding counseling during ANC, as well as the place and mode of delivery, were the factors that were strongly associated with suboptimal breastfeeding practice This current prevalence finding almost matches with research conducted in the Hadiya zone, which was 62.7 [21]. The results of this study are also per a study done in Gondar, northern Ethiopia, where the result was 64.4% [22].
On the other hand, the results of this study were lower than those of studies conducted in rural communities in the Jimma zone, Arjo district, which were 75% [24] and Gondar town northern Ethiopia,(80%) [19] respectively. In the former situation, this may be related to the socio-cultural differences in the environment, but in the latter case, the use of secondary data may have overestimated the prevalence of breastfeeding practice.
According to this study, fathers' education strongly indicates breastfeeding practice. The odds of practicing sub-optimal breastfeeding were therefore 2.23 times higher for women whose husbands had an informal education than mothers whose husbands had a higher level of education. The explanation might be that when the husband's educational level rises, so does communication between spouses concerning breastfeeding, and the husband may also support it. This result was in line with a study conducted in the Misha district, Hadiya zone, which found that mothers whose husbands had only a read-and-write educational background experienced a 60% decrease in optimal breastfeeding compared to those whose husbands had a college degree or higher [23]. Additionally, the study participants' knowledge and attitudes toward the best practices for breastfeeding were significantly associated with optimal breastfeeding. Accordingly, knowledgeable women had 77% lower odds of practicing sub-optimal breastfeeding than uninformed mothers. Similarly, mothers who did not believe that they were practicing optimal breastfeeding were 2.43 times more likely to do so than mothers who did. This might be explained by the fact that there is a higher likelihood of effective breastfeeding when women are more aware of it and perceive it to be beneficial. This finding is consistent with research done in Misha District Hadiya Zone [23], Jimma Town Southwest Ethiopia [24] Arbaminch Zuria Woreda [25], Hula District Sidama Zone [21], Gondar Town Northern Ethiopia [22]. This result is also consistent with research from the Gambia, where participants who reported positive attitudes had 2.4 times the odds of exclusively breastfeeding compared to those who reported negative attitudes [26] and from Anabra, Nigeria, where positive family attitudes were found to be significantly associated with exclusive breastfeeding (EBF) practice [27].
This current study found a statistically significant association between inadequate breastfeeding practices and breastfeeding counseling provided during ANC. As a result, participants in the study who did not receive breastfeeding counseling during ANC follow-up were two times more likely to have sub-optimal breastfeeding practice than their counterparts. This might be because ANC is the most crucial point of contact and the ideal moment to convey vital information about feeding infants and young children. This result was consistent with research from the Hadiya zone Misha district [24], Hula district Sidama zone [21], Debrebirhan town [28], and Gujarat region in India [29] found the association between breastfeeding counseling and breastfeeding practice.
Finally, the results of this study demonstrated a significant association between the modes of delivery and inadequate breastfeeding practice. This result was in line with research conducted in the northern Ethiopian town of Gondar, where study participants who had cesarean section deliveries were 59% less likely to breastfeed optimally than those who had vaginal deliveries [22]. This result was in line with a study from Jordan that found that mothers who had caesarian deliveries were more likely to practice inadequate breastfeeding than those who gave birth vaginally [30]. The stress and suffering brought by the surgery may cause inconvenient situations to start and continue optimal breastfeeding on time. Some data was not addressed by quantitative study. Therefore, we advise the next researcher to integrate qualitative research into their approach.
As a strength, this study was conducted in a community-based and utilized multi-stage sampling to incorporate candidate participants in the Gedeo Zone. However, it is not free from limitation, in this regard; a potential recall bias by the respondents might exist because the mothers were asked about their prior practices. We have tried to minimize potential recall bias by raising different probing questions.
The magnitude of sub-optimal breastfeeding among mothers was more than half (60%). Suboptimal breastfeeding practice was found to be significantly associated with factors like paternal education, maternal knowledge, attitude, breastfeeding counseling, and mode of delivery. Improving Healthcare professionals' counseling of pregnant mothers about the best ways of breastfeeding during ANC visits, deliveries, and postpartum care services was recommended. It is advised to use effective community-based behavior change communication to raise participants' awareness of and perceptions of the significance of optimal breastfeeding practice.
What is known about this topic
- Breastfeeding is a universal practice and isn't restricted to socio-economic background;
- Inadequate breastfeeding practices considerably raise the risk of all-cause mortality;
- Different social and personal barriers negatively affect the breastfeeding practice of mothers.
What this study adds
- Previously, most studies concentrated on a single aspect of breastfeeding practice; however, this study contributes to the communities' existing breastfeeding practices by developing a single composite measure - the breastfeeding performance index (BPI) - that takes into account all feeding practices as equally significant;
- This study assists stakeholders in adopting easy preventative intervention initiatives that address all aspects of breastfeeding practices.
The authors declare no competing interests.
Mahlet Birhane Estifanos had participated in the title selection, design, proposal preparation, statistical analysis, interpretation of results and manuscript preparation. Mihret Tesfu Legese, Ansha Seid Abegaz, Selamawit semagn Kebede, Gizaw Sisay, Hiwot Hailu Amare had participated in statistical analysis, interpretation of results and manuscript preparation. All the authors approved this manuscript to be published. All the authors have read and agreed to the final manuscript.
First and foremost, we would like to thank Dilla University College of Health science and medicine for granting us permission to carry out this study. Second, we want to thank the data collectors for being so steadfast in their efforts. Last but not least, we would like to express our gratitude to the study participants for their participation.
Table 1: sample size calculation for the second specific objective
Table 2: socio-demographic characteristics of study participants in Gedeo Zone southern Ethiopia, 2023
Table 3: socio-economic characteristics of households in Gedeo Zone southern Ethiopia, 2023
Table 4: obstetric and service-related factors of respondents in Gedeo zone southern Ethiopia, 2023
Table 5: knowledge-related characteristics of respondents in Gedeo Zone southern Ethiopia, 2023
Table 6: attitude related characteristics of respondents in Gedeo Zone southern Ethiopia, 2023
Table 7: logistic regression analysis result for factors associated with sub-optimal breastfeeding practice among children aged 6-12 months in Gedeo zone southern Ethiopia, 2023
- Berens P, Labbok M, Academy of Breastfeeding Medicine. ABM clinical protocol# 13: contraception during breastfeeding, revised 2015. Breastfeed Med. 2015 Jan-Feb;10(1):3-12. PubMed | Google Scholar
- Premani ZS, Kurji Z, Mithani Y. To explore the experiences of women on reasons in initiating and maintaining breastfeeding in urban area of Karachi, Pakistan: An exploratory study. ISRN Pediatr. 2011;2011:514323. PubMed | Google Scholar
- Koosha A, Hashemifesharaki R, Mousavinasab N. Breast-feeding patterns and factors determining exclusive breast-feeding. Singapore Med J. 2008 Dec;49(12):1002-6. PubMed | Google Scholar
- Taslima A, Sujan MD, Paul DK, Ahmed T, Gulshan R, Juliana F et al. Impact of Infant and Young Child Feeding (IYCF) Counseling on Practices and Knowledge of Mothers in Rural Areas. World Journal of Nutrition and Healt 2019;7(1):11-17.
- Chantry CJ, Eglash A, Labbok M. Position on breastfeeding-revised 2015. Breastfeed Med. 2015 Nov;10(9):407-11. PubMed | Google Scholar
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013 Aug 3;382(9890):427-451. PubMed | Google Scholar
- Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC et al. Why invest, and what it will take to improve breastfeeding practices. Lancet. 2016 Jan 30;387(10017):491-504. PubMed | Google Scholar
- Brady JP. Marketing breast milk substitutes: problems and perils throughout the world. Arch Dis Child. 2012 Jun;97(6):529-32. PubMed
- Roberts T, Carnahan E, Gakidou E. Burden attributable to suboptimal breastfeeding: a cross-country analysis of country-specific trends and their relation to child health inequalities. The lancet. 2013 Jun 17;381:S126. Google Scholar
- World Health Organization. Exclusive Breast Feeding for Six Months Best for Babies Every Where. January 15, 2011. Accessed November 15, 2023.
- Elizabeth KE. Feeding of young infants and children in exceptionally difficult circumstances (like, HIV and humanitarian emergencies). Solution exchange MCH Community Newsletter Breastfeeding Month Special. 2008. Google Scholar
- UNICEF W. Tracking progress for breastfeeding policies and programmes: global breastfeeding scorecard 2017. Geneva, Switzerland: World Health Organization; 2017. Google Scholar
- World Health Organization. Early Initiation of breastfeeding: The key to survival and beyond. Breastfeeding is today the single most effective preventive intervention for improving the survival and health of children”. WHO Secretariat. June 2010.
- Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J et al. Optimal breastfeeding practices and infant and child mortality: a systematic review and meta-analysis. Acta Paediatr. 2015 Dec;104(467):3-13. PubMed | Google Scholar
- WHO U. Global nutrition targets 2025: breastfeeding policy brief (WHO/NMH/NHD14. 7). Geneva: World Health Organization; 2014. Google Scholar
- Wu H, Zhao M, Magnussen CG, Xi B. Global prevalence of WHO infant feeding practices in 57 LMICs in 2010-2018 and time trends since 2000 for 44 LMICs. EClinicalMedicine. 2021 Jul 6:37:100971. PubMed | Google Scholar
- Tessema M, Belachew T, Ersino G. Feeding patterns and stunting during early childhood in rural communities of Sidama, South Ethiopia. Pan Afr Med J. 2013 Feb 26;14:75. PubMed | Google Scholar
- Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. 2016.
- Haile D, Biadgilign S. Higher breastfeeding performance index is associated with lower risk of illness in infants under six months in Ethiopia. Int Breastfeed J. 2015 Nov 27;10:32. PubMed | Google Scholar
- Gedeo zone health office report. Gedeo, Ethiopia; 2018.
- Hoche S, Meshesha B, Wakgari N. Sub-optimal breastfeeding and its associated factors in rural communities of Hula District, southern Ethiopia: a cross-sectional study. Ethiop J Health Sci. 2018 Jan;28(1):49-62. PubMed | Google Scholar
- Nigatu YT, Worku N. Optimal breastfeeding practice and associated factors amongst working mothers. East African Journal of Public Health. 2014 Sep 19;11(1):704-15. Google Scholar
- Abageda M, Mokonen A, Hamdela B. Predictors of Optimal Breastfeeding Practices Among Mothers Who Have Less Than 24 Months of Age Children in Misha District, Hadiya Zone, South Ethiopia. J Preg Child Health. 2015;2:182. Google Scholar
- Tamiru D, Belachew T, Loha E, Mohammed S. Sub-optimal breastfeeding of infants during the first six months and associated factors in rural communities of Jimma Arjo Woreda, Southwest Ethiopia. BMC Public Health. 2012 May 18;12:363. PubMed | Google Scholar
- Tamiru D, Tamrat M. Constraints to the optimal breastfeeding practices of breastfeeding mothers in the rural communities of Arba Minch Zuria Woreda, Ethiopia: a community-based, cross-sectional study. South African Journal of Clinical Nutrition. 2015;28(3):134-9. Google Scholar
- Senghore T, Omotosho TA, Ceesay O, Williams DCH. Predictors of exclusive breastfeeding knowledge and intention to or practice of exclusive breastfeeding among antenatal and postnatal women receiving routine care: a cross-sectional study. Int Breastfeed J. 2018 Mar 2;13:9. PubMed | Google Scholar
- Ukegbu AU, Ukegbu PO, Onyeonoro UU, Ubajaka CF. Determinants of breastfeeding patterns among mothers in Anambra State, Nigeria. South African Journal of Child Health. 2011;5(4):112-6. Google Scholar
- Gultie T, Sebsibie G. Determinants of suboptimal breastfeeding practice in Debre Berhan town, Ethiopia: a cross sectional study. Int Breastfeed J. 2016 Mar 22;11:5. PubMed | Google Scholar
- Chudasama RK, Patel PC, Kavishwar AB. Determinants of exclusive breastfeeding in south Gujarat region of India. J Clin Med Res. 2009 Jun;1(2):102-8 PubMed | Google Scholar
- Khassawneh M, Khader Y, Amarin Z, Alkafajei A. Knowledge, attitude and practice of breastfeeding in the north of Jordan: a cross-sectional study. Int Breastfeed J. 2006 Sep 23;1:17. PubMed | Google Scholar