Hepatitis B virus prevalence and its genotypic association with drug resistance in HBV/HIV co-infected patients in Western Kenya: a cross-sectional study
Bernard Wandera Onyango, David Onyango Miruka, Stanslaus Kiilu Musyoki
Corresponding author: Bernard Wandera Onyango, Maseno University, School of Physical and Biological Sciences, Department of Zoology, Kisumu, Kenya 
Received: 21 Jul 2023 - Accepted: 16 Sep 2023 - Published: 16 Apr 2024
Domain: Molecular Biology,Virology,Laboratory medicine
Keywords: Hepatitis B, HIV, co-infection, polymerase gene mutation, drug resistance
©Bernard Wandera Onyango et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Bernard Wandera Onyango et al. Hepatitis B virus prevalence and its genotypic association with drug resistance in HBV/HIV co-infected patients in Western Kenya: a cross-sectional study. PAMJ-One Health. 2024;13:14. [doi: 10.11604/pamj-oh.2024.13.14.41157]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/13/14/full
Research 
Hepatitis B virus prevalence and its genotypic association with drug resistance in HBV/HIV co-infected patients in Western Kenya: a cross-sectional study
Hepatitis B virus prevalence and its genotypic association with drug resistance in HBV/HIV co-infected patients in Western Kenya: a cross-sectional study
![]() Bernard Wandera Onyango1,&,
Bernard Wandera Onyango1,&, ![]() David Onyango Miruka1,
David Onyango Miruka1, ![]() Stanslaus Kiilu Musyoki2
Stanslaus Kiilu Musyoki2
&Corresponding author
Introduction: the prevalence of co-infections involving hepatitis B and the renowned human immunodeficiency viruses is alarmingly widespread, largely due to the shared transmission pathways. However, it is disheartening to note the lack of dedicated research on this comorbidity in Western Kenya, despite the region's high prevalence of HIV. Hence, the present investigation focuses on ascertaining the prevalence of Hepatitis B, identifying its genotypes, and exploring its polymerase gene mutation patterns responsible for drug resistance among individuals with HIV in the region.
Methods: this cross-sectional study encompassed a comprehensive evaluation of individuals receiving HIV care at the renowned Jaramogi Oginga Odinga Teaching and Referral Hospital. Their Hepatitis B status was determined, DNA extracted, and the viral load quantified. The Polymerase gene was amplified, sequenced, and compared with the existing databases confirming the genotype and polymerase gene mutations. Data was meticulously entered into an Excel spreadsheet and analyzed using SPSS.
Results: most participants were on Tenofovir, Lamivudine, and dolutegravir. Hepatitis B was detected in 5.4% of the participants, all genotype A. Further analysis revealed specific HBV polymerase gene mutations causing drug resistance among some participants who were on treatment. There was a statistically significant association between Hepatitis B genotype A and polymerase gene-drug resistance mutations, with a p-value of 0.025.
Conclusion: the comorbidity rate is 5.4%, whereas the prevailing genotype is A, subtype A1. There is a notable correlation between Hepatitis B genotype A and the presence of drug resistance mutations rtT184S, rtM204V, rt204I, and rtL180M.
Hepatitis B virus (HBV) is a type of virus that can make people sick. It is found in the Hepadnaviridae family and affects the liver. It was first discovered in a group of people called the Australian Aborigines [1]. After entering the liver cells, the virus makes a special type of DNA called covalently closed circular DNA (cccDNA). This DNA helps the virus to multiply and stay in the body for a long time [1,2]. Hepatitis B virus (HBV) has ten different types, [3] and it can be passed from a mother to her baby or through things like having unprotected sex, sharing needles, or getting a blood transfusion. HIV is a type of RNA virus that belongs to the Retroviridae family and the Lentivirus genus [4]. There exist two prominent variants of HIV, namely HIV 1 and HIV 2, which are responsible for causing the global Acquired Immunodeficiency Syndrome (AIDS) pandemic [5]. These viruses were originally transmitted from non-human primates to humans and have since evolved into different groups and subtypes [5]. HIV-1 has four groups (M, O, N, and P) and nine subtypes (A-D, F-H, J, K), while HIV-2 has nine subgroups (A-I) but only subgroups A and D are currently circulating [4]. The virus is made up of RNA molecules and three viral enzymes, as well as various proteins. HIV-2 is primarily found in West Africa, while the distribution of HIV-1 subtypes varies in different regions of the world [4,5].
The prevalence of HBV/HIV co-infection is strikingly pronounced, with shared entry points such as the bloodstream, sexual pathway, and mother-to-child transmission being contributing factors [6]. In the treatment of chronic HBV in individuals with HIV co-infection, the utilization of a first-generation nucleos(t)ide analog, namely Lamivudine (3TC), or its combination therapy, has led to elevated levels of HBV 3TC resistance. Furthermore, this resistance extends to other agents like Emtricitabine and Entecavir, thus posing additional according to Archampong et al. and Spearman et al. [7-9]. When someone has both HBV and HIV, it can make it harder for their body to get rid of HBV. It can also make the HBV virus multiply faster and cause more liver problems. Having both viruses can also make HIV get worse more quickly and make it harder for HIV treatment to work. This can lead to different health issues like liver problems from the medications and problems with the immune system, according to National AIDS & STI Control Program [10].
In the realm of health, it is crucial to acknowledge the significant disparities faced by individuals living with HIV. Astonishingly, research indicates that HIV-positive individuals are confronted with a staggering 40% higher likelihood of contracting HBV infection compared to their HIV-negative counterparts [11]. Moreover, in regions where the prevalence of this infection is alarmingly high, approximately 10% of those living with HIV also bear the burden of HBV infection [12]. This comorbidity, undeniably, amplifies the risks of both morbidity and mortality among HIV patients, emphasizing the urgent need for heightened attention and intervention [11]. As per the esteemed [13], HBV and HIV have been identified as the prevailing chronic co-morbidities globally, owing to a shared means of entry. However, it is disheartening to note the lack of dedicated research on this particular comorbidity in Western Kenya, despite the region's high prevalence of HIV. Hence, the present investigation focuses on ascertaining the prevalence of Hepatitis B, identifying its genotypes, and exploring its polymerase gene mutation patterns responsible for drug resistance among individuals with HIV in the region.
The objective of this study was to present investigation focuses on ascertaining the prevalence of Hepatitis B, identifying its genotypes, and exploring its polymerase gene mutation patterns responsible for drug resistance among individuals with HIV in the region. Research questions: what is the prevalence of HBV/HIV co-infection in Western Kenya?
The study design: this study employed a descriptive cross-sectional design in a hospital setting.
Setting: the study was conducted at Jaramogi Oginga Odinga Teaching and Referral Hospital (JOOTRH), a renowned hospital nestled in Kisumu, Western Kenya between April 2022 and July 2022. Situated 1131 meters above sea level, with coordinates of 0°6' S and 34°45' E, this location basks in the delight of abundant sunshine throughout the year. Notably, the hospital houses a remarkable Patient Support Centre (PSC), catering to HIV-positive patients and serving as a pivotal hub for various support amenities in the western region. It is worth mentioning that the Kisumu County hospital catchment region, where our study was conducted, boasts a staggering HIV prevalence rate of 17.5% (as of 2022), surpassing the national average of 4.8%. Therefore, our selection of this facility holds immense significance.
Participants: the study encompassed individuals of every gender, who have tested positive for HIV. We took into account patients across various age groups, including minors aged 0 to 14, individuals aged 15 to 47, middle-aged individuals aged 48 to 63, and the elderly aged 64 and above. Both those receiving antiretroviral therapy (ART) and those who have not yet started treatment were included, as long as they expressed their consent, showed willingness to participate, and were open to providing a blood sample.
Variables: the presence of HIV, the presence of HBV, and the course of treatment are all independent variables in this study. The polymerase gene mutations and drug resistance are the dependent variables.
Data sources/measurement
The collection of blood samples: four milliliters (4 ml) of whole blood was drawn from the participant's arm in ethylene diamine tetraacetic acid (EDTA) vacutainer tubes using the World Health Organization (WHO) recognized standard operating procedure for the venipuncture technique [14]. The samples were centrifuged at 3500 RPM (Hettich Lab Technology™ ROTOFIX 32 A Benchtop Centrifuge-Germany) for 5 minutes, and plasma was aliquoted into 2ml cryovials. Samples were carefully triple packed, and transferred to the research Lab at Maseno University, where they were frozen at -20° C awaiting analysis.
Serological determination of the HBV status: after reaching the necessary number of samples, the plasma underwent screening for the hepatitis B surface antigen (HBsAg) indicator using a highly efficient one-step HBsAg rapid test (Bioline SD HBsAg WB), following the prescribed protocol. The plasma samples were carefully thawed to a temperature of 25 degrees Celsius before conducting the test. The testing device was delicately taken out of its protective foil packaging and positioned on a clean and even surface. In order to maintain accuracy, each testing device was labeled with the corresponding patient identifier. Using a precise micropipette, exactly 100μl of plasma was dispensed into the designated specimen well labeled as "S". To ensure reliability, positive and negative control samples were simultaneously tested alongside the actual samples, and the results were accurately interpreted after a waiting period of 20 minutes.
The extraction of HBV genomic DNA: we employed Qiagen's esteemed kit from Germantown to carefully extract the HBV DNA from seropositive plasma samples, meticulously adhering to the manufacturer's guidelines. In a concise summary, the initial step entailed the gentle lysis of 200μl of plasma sample with the addition of 20μl Proteinase K, subsequently undergoing an incubation period at 70° C. Subsequently, the proteins were skillfully precipitated in 200μl of 96% ethanol, meticulously progressing through the binding, washing, elution via a sophisticated spin protocol employing reaction buffer.
HBV viral load detection and quantification: the HBV viral load was accurately measured using the advanced Rotor-Gene Q -5 plex HRM system from Qiagen, in conjunction with the highly reliable RealStar® HBV PCR Kit 2.0 from Germany. The procedure involved precise steps, including the addition of 5μl of Master A, 20μl of Master B, and 2.5μl of Internal Control (IC), resulting in a reaction volume of 50μl when combined with 25μl of the sample. It is important to note that the Limit of Detection (LOD) for the HBV Genotype is set at a minimum of >3000 IU/mL, ensuring accurate and sensitive detection of the virus.
Amplification of HBV DNA through the real-time polymerase chain reaction: a section of the HBV pol gene covering 1230bp with viral load >3000 IU/mL was amplified by real-time polymerase chain reaction (RT-PCR) on Applied Biosystem Veriti - Thermal Cycler (USA). Briefly, 12.5μl of Takara Premix Ex Taq Master Mix (2X) was combined with 1μl of Primer HBV F1 5´- CTGCTGGTGGCTCCAGTT-3´ (10p mol), 1μl of Primer HBV R1 5´-GCTAGGAGTTCCGCAGTATGG -3´ (10p mol), 7.5 of WFI (water for injection), and 3μl of DNA Sample making the final reaction volume of 25μl. The thermal cycling conditions were programmed as follows: In step one, 1 cycle at 950 C for 10 min. In step two, 35 cycles at 95° Celsius for 30 sec, 56° Celsius for 40 sec, and 72° Celsius for 1 min. In step three, 1 cycle of hold at 37° Celsius. Analysis of the PCR products was done on Bio-Rad Agarose Gel Electrophoresis Unit (Figure 1).
Sequencing: the polymerase gene sequencing was carefully carried out on a state-of-the-art 3500 Dx Series Genetic Analyzer, manufactured by Thermo Fisher Scientific in the United States. This process involved entrusting the direct Sanger Sequencing to the esteemed UNIPATH SPECIALTY Laboratory in India. To successfully accomplish this task, we utilized the HBV GP FP 5´- TTCTTAGCGTATTGGAGCTCCTGCTGGTGGCTCCAGTT- 3´ and HBV GP RP 5´- AAGTATCAGTATTGCGTTGTTGCTAGGAGTTCCGCAGTATGG- 3´ primers during the sequencing PCR.
Sequence analysis and genotyping: the consensus sequences were carefully crafted using the sophisticated CodonCode aligner software. In this process, the esteemed reference sequence from National Council for Biotechnology Information (NCBI) was seamlessly integrated into the software, alongside the invaluable test sequence data. The alignment of the test sequences with the reference sequence resulted in the creation of exquisite contigs, which were subsequently elegantly exported in the revered FASTA file format. To further enhance our results and credibility, a Nucleotide BLAST was conducted on our HBV sequences, allowing us to procure a profoundly harmonious sequence from the esteemed NCBI, thereby decisively confirming the HBV Genotypes and subtypes.
Drug resistance prediction: the Geno2Pheno website was utilized to identify polymerase gene mutations associated with drug resistance, as well as to correlate with the genotype of the provided sequences. To accomplish this, the sequences were uploaded to the website in the FASTA file format. The results were carefully analyzed and presented in a user-friendly output window, and subsequently exported in a CSV file format for further analysis. Notably, the drugs Lamivudine, Adefovir, Entecavir, Tenofovir DF, and Telbivudine were subjected to testing.
Bias: the study employed consecutive sampling, also known as the total enumerative sampling approach, ensuring that all individuals who met the inclusion criteria were carefully selected to participate in the research. By seamlessly integrating this process into the clinic's routine operations, we were able to efficiently recruit enough participants from individuals visiting the clinic to seek HIV care until our desired sample size was achieved. They completed the informed consent form as part of the ethical requirements and then recruited. To gather information on these patients, their medical records were meticulously reviewed by the medical records officer. The study nurse, carefully chosen by the nursing officer in charge, then recruited the participants. Data was gathered from both individuals with prior experience in antiretroviral therapy (ART) and those who were new to this treatment, all of whom were seeking assistance at the esteemed JOOTRH patient support center. This was encouraged in an effort to combat bias.
Study size: the determination of the sample size was meticulously carried out by considering various factors such as the standard normal variate, the anticipated prevalence in the population based on prior research, and the absolute error as stated by Charan J et al. [15].
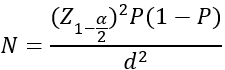
Where, N = sample size Z1-α/2 = standard normal variate [at 5% type 1 error (P<0.05), it is 1.96] P = Expected prevalence/ proportion in the population based on previous studies d = Absolute error/precision The occurrence (P) of HBV-HIV co-infection is estimated at a remarkable 5.7% nationally, Z1-α/2 is 1.96 and d is 5%. Therefore,
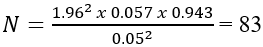
Moreover, an impressive total of 93 samples were meticulously utilized for the purpose of this study, surpassing the obligatory minimum sample size of 83, thereby significantly enhancing the robustness and reliability of the obtained outcomes.
Statistical analysis: the information for each participant was carefully recorded in a refined Excel spreadsheet, capturing essential details such as age, gender, treatment plan, and date of sample collection. Additionally, the participants' HBV and drug resistance statuses were carefully noted. The data underwent thorough verification and consistency checks and was subsequently analyzed using the highly regarded IBM SPSS version 20. The prevalence of co-infection between the two viruses was presented in percentage. To investigate the correlation between HBV genotypes and the presence or absence of drug-resistance mutations in individuals undergoing Lamivudine combination therapy, the Chi-square test of association was employed. This two-tailed test considered a p-value ≤ 0.05 as statistically significant.
Ethical consideration and informed consent: this research study was granted initial approval by the esteemed School of Graduate Studies (SGS) of Maseno University, demonstrating their recognition of its significance. Furthermore, the study protocol received ethical approval from the respected Institutional Ethical Review Committee (IERC) JOOTRH, emphasizing the commitment to conducting this research in a responsible and morally sound manner. In addition, the National Commission for Science Technology and Innovation (NACOSTI) granted their approval, further validating the importance and validity of this study, as indicated by license number NACOSTI/P/22/16151. The chief executive officer at JOOTRH, recognizing the value of this research, provided administrative consent before the commencement of data collection at the PSC. Every participant involved in the study provided their explicit written assent and informed consent, ensuring their willingness and understanding of their involvement. For younger participants, who may not have been able to provide written consent, an assent was obtained under the guidance of parents/guardians. The utmost care was taken to ensure the confidentiality of the participants by conducting the necessary procedures privately and explaining the process to the participants. To further protect their identity, unique identifiers were assigned to each participant for the duration of the study. Participants were also explicitly told of their right to decline at any point, ensuring their autonomy and comfort throughout the research process.
Sociodemographic information and clinical features of the study participants: the study included a diverse group of 93 individuals across different age groups, including those below 15 years, between 15 and 47 years, between 48 and 63 years, and above 64 years. The study found an average age of 34.12 years and the median age was 34.00 years. In terms of gender, the study found an equally fair representation, with 41 males (41.1%) and 52 females (55.9%) participating. It is important to note that younger participants made up a small percentage of the total (6.5%), while the majority (80.6%) fell within the 15-47 age range. Participants between 48 and 63 years accounted for 8.6%, while those above 64 years constituted 4.3%. In terms of medication usage, the study found that the majority (96.8%) were on antiretroviral therapy (ART). Specifically, 73 individuals (78.5%) were prescribed the Tenofovir (TDF) - Lamivudine (3TC) - Dolutegravir (DTG) combination, which is considered highly effective. Additionally, 17 participants (18.3%) were receiving tenofovir disoproxil, lamivudine, and dolutegravir (TLD), another recognized therapy option. Only a small subset of 3 individuals (3.2%) were not currently undergoing any form of therapy (Table 1).
The electrophoretic analysis of HBV PCR amplicons: the PCR products were observed using an Ultraviolet (UV) trans-illuminator from ultraviolet photoelectron (UVP), renowned for its exceptional quality and precision (Figure 1).
HBV/HIV co-morbidity rate, HBV genotype and polymerase drug resistance mutations: from a cohort of 93 individuals living with HIV, 5 individuals (5.4%) were discovered to exhibit positivity for HBsAg. On polymerase gene sequencing and sequence analysis, HBV genotype A, subtype A1 was identified. Further analysis of the sequences revealed drug resistance mutation patterns at certain positions of the polymerase gene labeled as rtT184S, rtM204V, rt204I, and rtL180M. This study also revealed a noteworthy correlation (p-value of 0.025) between HBV genotype A and the development of drug resistance in individuals who have undergone previous treatment with Lamivudine combination therapy (Table 2)
The prevalence of Hepatitis B and HIV co-morbidity in Western Kenya: the research results indicate that Hepatitis B is widespread among individuals who are HIV-positive, as a result of shared avenues of transmission, common risk factors, and geographic prevalence. Comorbidity of these two viruses has been shown to result in higher rates of illness and mortality compared to infections caused by either HBV or HIV alone. This study specifically identified a prevalence of HBV/HIV co-infection at 5.4%, aligning with previous research conducted in Kenya. Notably, the burden of infection was found to be higher among female participants than male participants, although the reasons for this disparity remain unclear. However, it is important to acknowledge that this prevalence contributes to the suboptimal treatment outcomes and drug resistance observed within this patient population.
Hepatitis B virus Genotypes at Jaramogi Oginga Odinga Teaching and Referral Hospital, Western Kenya: this study employed the sophisticated Codon Code aligner software to determine HBV genotypes by generating Consensus Sequences. By aligning numerous nucleotide sequences with comparable functions, the most prominently expressed nucleotide was identified at each location, resulting in the creation of a consensus sequence. These conserved sequences often signify a shared function or binding domain. The obtained sequences were meticulously scrutinized by conducting a sophisticated BLAST analysis on the esteemed NCBI platform. This comprehensive comparison allowed us to identify and authenticate the presence of homologous sequences within the same genomic region, thereby validating the HBV Genotypes. Remarkably, each and every sequence that was examined unequivocally belonged to the highly prevalent HBV genotype A, specifically subtype A1.
Correlation of Hepatitis B virus genotype A with drug resistance: this study has revealed a noteworthy correlation (p value= 0.025) between HBV genotype A and the development of drug resistance in individuals who have undergone previous treatment. However, it is important to note that no drug resistance mutations were observed in relation to Tenofovir and Adefovir, as well as in the treatment naïve subjects, aligning with findings from other studies on HBV drug resistance [16].
Limitations: the most pressing challenge faced throughout the duration of this study was the regrettably inadequate financial resources at our disposal. Studies involving sequencing necessitate ample financial resources to obtain reliable data from next-generation sequencing, a requirement that was not adequately met in this particular instance as the majority of the study's objectives were funded personally, an arrangement that proved insufficient. Additionally, the limited sample size presents a further constraint, potentially hampering the ability to accurately represent the entire region under study. However, caution should be exercised when generalizing the results to the broader Kenyan population or individuals not afflicted with HIV.
Interpretation: considering the consistent findings across multiple studies conducted in Kenya and the region, we can confidently conclude that the null hypothesis, which suggests no difference in HBV/HIV co-infection rates at JOOTRH and other parts of Kenya, cannot be rejected. The outcomes of this investigation align with previous studies conducted both within Kenya and the wider region. For instance, a study carried out at Mama Lucy Hospital in Nairobi, Kenya, in 2016 recorded a prevalence of 5.5 percent [17], while a study in Eldoret documented a prevalence of 5.7 percent [18]. Similarly, studies conducted in Northwest Ethiopia in 2017 found a co-infection rate of 5.5% based on the study according to Deressa T et al. [8] postulation, and Uganda reported a comorbidity rate of 6.7% according to Ocama P et al. [19]. Likewise, a study conducted in Tanzania revealed a co-infection rate of 6.6 percent [20].
When it comes to HBV genotypes, the results of this study align with previous research conducted in Nairobi and the coastal region, which consistently reported the high prevalence of HBV genotype A. For example, a study conducted by Ochwoto M et al. [21] among jaundice patients in Kenya revealed that genotypes A and D were the prevailing strains, further reinforcing our findings. The findings align with similar research conducted in neighboring countries. For example, a study in Tanzania revealed that HBV genotype A was present in a significant 86.1% of HIV-infected participants [22]. Similarly, a genotypic study among blood donors in Ethiopia demonstrated that HBV genotype A was the predominant strain, accounting for 68.2% of cases [23]. Additionally, a separate genotypic study conducted in Rwanda among blood donors from various transfusion centers revealed a uniformity of isolates belonging to genotype A, specifically subtype A1 [24]. Through the meticulous construction of a sophisticated phylogenetic tree, we were able to authenticate the genotypes with utmost certainty, illuminating the intricate evolutionary connections between the taxa. Our diligent efforts involved aligning our sequences with those sourced from various countries in East Africa, expanding our scope to encompass more African countries, and even extending to select nations across the globe, as per the esteemed work of Lin CL et al. [3]. The culmination of our diligent research unequivocally affirms that the prevailing HBV genotype in Western Kenya remains the steadfast HBV genotype A subtype A1.
The emergence of drug resistance mutations, particularly in relation to Lamivudine and the subsequent cross-resistance to other agents, occurs when Methionine in the tyrosine methionine aspartate (YMMD) catalytic site motif is replaced by valine, leucine, or serine [25,26]. Each resistance mutation is believed to induce specific structural changes in the polymerase, preventing the incorporation of Nucleos(t)ide Analogues into replicating DNA [27]. Furthermore, it is worth noting that there were no polymerase gene resistance mutations detected in the treatment-naïve participants who were co-infected with HBV and HIV, consistent with previous research findings [7]. The notable resistance mutations identified in the polymerase were rtM204V, rt204I, rtL180M, and rtV173L.
Generalisability: it is important to note that this study was conducted at the main tertiary teaching and referral center in Kisumu, catering to a significant portion of Western Kenya. Therefore, these results can be generalized to the broader Kenyan population of individuals afflicted with HBV/HIV. The results can also be generalized to the wider East African region from the consistency and correlation of the findings from selected studies in the region.
The overall comorbidity rate for HBV and HIV at Jaramogi Oginga Odinga Teaching and Referral Hospital in Western Kenya is 5.4%. According to the study, genotype A, subtype A1 of HBV continues to be the predominant genotype in circulation in Western Kenya and across Kenya. The study also found a strong correlation between the drug resistance mutations rtT184S, rtM204V, rt204I, and rtL180M and HBV genotype A. (p=0.025). The available data strongly indicates a pressing need for extensive and meticulously planned prospective studies that thoroughly explore the occurrence of HBV in HIV-infected people in the region. Additionally, it is imperative to conduct HBV genotyping and sequencing to identify drug-resistance mutations, thus ensuring optimal patient care. We earnestly implore the government, in collaboration with NASCOP, and our esteemed funding partners to actively prioritize and invest resources in the provision of comprehensive HBV care for individuals co-infected with HIV.
What is known about this topic
- That there are different HBV genotypes;
- Genotype A of HBV is predominant in Kenya.
What this study adds
- From a cohort of 93 individuals living with HIV, 5 individuals (5.4%) were discovered to exhibit positivity for HBsAg. On polymerase gene sequencing and sequence analysis, HBV genotype A, subtype A1 was identified. Further analysis of the sequences revealed drug resistance mutation patterns at certain positions of the polymerase gene labeled as rtT184S, rtM204V, rt204I, and rtL180M;
- This study also revealed a noteworthy correlation (p-value of 0.025) between HBV genotype A and the development of drug resistance in individuals who have undergone previous treatment with Lamivudine combination therapy;
- The study further revealed that there is cross-resistance between Lamivudine, Telbivudine, and Entecavir drugs among individuals with HBV/HIV comorbidity.
The authors declare no competing interest.
Bernard Wandera Onyango: conceived of the presented idea, developed the theory, performed the computations and discussed the results and wrote the final manuscript. David Onyango Miruka: supervised the findings of this work and contributed to the final manuscript. Stanslaus Kiilu Musyoki: supervised the findings of this work and contributed to the final manuscript. All the authors have read and agreed to the final manuscript.
We would like to thank Dr. Sunder Raj Rao of Jalaram Medical Services for his immense support during the sample analysis, Dr. Neeraj Arora for his commitment to supporting sample analysis; and the entire Unipath Specialty Laboratory Ahmedabad team for the technical expertise. Thanks to Janet Atieno of Jaramogi Oginga Odinga Teaching and Referral Hospital patient support center (PSC) and her team for their immense support during sample collection, and all the PSC study participants.
Table 1: sociodemographic and clinical characteristics of the study participants
Table 2: analysis results of sequences using the max planck institute data base
Figure 1: A) agarose gel electrophoresis; B) agarose gel electrophoresis
- Tsukuda S, Watashi K. Hepatitis B virus biology and life cycle. Antiviral Res. 2020 Oct;182:104925. PubMed | Google Scholar
- Seeger C, Mason WS. Molecular biology of hepatitis B virus infection. Virology. 2015;479-480:672-686. PubMed | Google Scholar
- Lin CL, Kao JH. Hepatitis B virus genotypes and variants. Cold Spring Harb Perspect Med. 2015 May 1;5(5):a021436. PubMed | Google Scholar
- Bivigou-Mboumba B. Human Immunodeficiency Virus-Hepatitis B Virus (HIV-HBV) Coinfection. Advances in HIV and AIDS Control. 2018 Dec 12. Google Scholar
- Bbosa N, Kaleebu P, Ssemwanga D. HIV subtype diversity worldwide. Curr Opin HIV AIDS. 2019 May;14(3):153-160. PubMed | Google Scholar
- Yousif M, Mudawi H, Hussein W, Mukhtar M, Nemeri O, Glebe D et al. Genotyping and virological characteristics of hepatitis B virus in HIV-infected individuals in Sudan. Int J Infect Dis. 2014 Dec:29:125-32. PubMed | Google Scholar
- Archampong TNA, Boyce CL, Lartey M, Sagoe KW, Obo-Akwa A, Kenu E et al. HBV genotypes and drug resistance mutations in antiretroviral treatment-naive and treatment-experienced HBV-HIV-coinfected patients. Antivir Ther. 2017;22(1):13-20. PubMed | Google Scholar
- Deressa T, Damtie D, Fonseca K, Gao S, Abate E, Alemu S et al. The burden of hepatitis B virus (HBV) infection, genotypes and drug resistance mutations in human immunodeficiency virus-positive patients in Northwest Ethiopia. PLoS One. 2017 Dec 27;12(12):e0190149. PubMed | Google Scholar
- Spearman CW, Afihene M, Ally R, Apica B, Awuku Y, Cunha L et al. Hepatitis B in sub-Saharan Africa: strategies to achieve the 2030 elimination targets. Lancet Gastroenterol Hepatol. 2017 Dec;2(12):900-909. PubMed | Google Scholar
- National AIDS & STI Control Program. Guidelines on Use Antiretroviral Drugs for Treating and preventing HIV infection in Kenya. 2018. Accessed on July 21, 2023.
- Weldemhret L. Epidemiology and Challenges of HBV/HIV Co-Infection Amongst HIV-Infected Patients in Endemic Areas: Review. HIV AIDS (Auckl). 2021 May 5:13:485-490. PubMed | Google Scholar
- Cheng Z, Lin P, Cheng N. HBV/HIV Coinfection: Impact on the Development and Clinical Treatment of Liver Diseases. Front Med (Lausanne). 2021 Oct 4:8:713981. PubMed | Google Scholar
- World Health Organisation. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021. 2021. Accessed on July 21, 2023.
- World Health Organization. WHO guidelines on drawing blood: best practices in phlebotomy. World Health Organization; 2010. PubMed | Google Scholar
- Charan J, Biswas T. How to calculate sample size for different study designs in medical research. Indian Journal of Psychological Medicine. 2013;35(2):121-126. PubMed | Google Scholar
- Jia HH, Li KW, Chen QY, Wang XY, Harrison TJ, Liang SJ et al. High Prevalence of HBV Lamivudine-Resistant Mutations in HBV/HIV Co-Infected Patients on Antiretroviral Therapy in the Area with the Highest Prevalence of HIV/HBV Co-Infection in China. Intervirology. 2018;61(3):123-132. PubMed | Google Scholar
- Mabeya SN, Ngugi C, Nyamache AK, Lihana R. Prevalence of HepatitisB virus infections among HIV infected individuals in Nairobi, Kenya. East African Medical Journal. 2016;93(6):221-5. Google Scholar
- Wambani RJ, Ogola PE, Makori AW, Nyamai DW, Lihana R, Burugu MW. Hepatitis B and C Co-Infections among HIV-1 Infected Patients Attending the Academic Model Providing Access to Healthcare Clinic, Kenya, 2014. J Infect Dis Diagn. 2015;1(102):2. Google Scholar
- Ocama P, Seremba E, Apica B, Opio K. Hepatitis b and HIV co-infection is still treated using lamivudine-only antiretroviral therapy combination in Uganda. Afr Health Sci. 2015 Jun;15(2):328-33. PubMed | Google Scholar
- Kilonzo SB, Gunda DW, Kashasha F, Mpondo BC. Liver fibrosis and Hepatitis B coinfection among ART Naive HIV-infected patients at a tertiary level hospital in Northwestern Tanzania: A cross-sectional study. J Trop Med. 2017:2017:5629130. PubMed | Google Scholar
- Ochwoto M, Kimotho JH, Oyugi J, Okoth F, Kioko H, Mining S et al. Hepatitis B infection is highly prevalent among patients presenting with jaundice in Kenya. BMC Infect Dis. 2016 Mar 1:16:101. PubMed | Google Scholar
- Kilonzo SB, Gunda DW, Mpondo BCT, Bakshi FA, Jaka H. Hepatitis B Virus Infection in Tanzania: Current Status and Challenges. J Trop Med. 2018 Jan 30:2018:4239646. PubMed | Google Scholar
- Ambachew H, Zheng M, Pappoe F, Shen J, Xu Y. Genotyping and sero-virological characterization of hepatitis B virus (HBV) in blood donors, Southern Ethiopia. PLoS One. 2018 Feb 20;13(2):e0193177. PubMed | Google Scholar
- Twagirumugabe T, Swaibu G, Walker TD, Lindh M, Gahutu JB, Bergström T et al. Hepatitis B virus strains from Rwandan blood donors are genetically similar and form one clade within subgenotype A1. BMC Infect Dis. 2017 Jan 6;17(1):32. PubMed | Google Scholar
- Mokaya J, McNaughton AL, Hadley MJ, Beloukas A, Geretti AM, Goedhals D et al. A systematic review of hepatitis B virus (HBV) drug and vaccine escape mutations in Africa: A call for urgent action. PLoS Negl Trop Dis. 2018 Aug 6;12(8):e0006629. PubMed | Google Scholar
- Shaw T, Bartholomeusz A, Locarnini S. HBV drug resistance: Mechanisms, detection and interpretation. J Hepatol. 2006 Mar;44(3):593-606. PubMed | Google Scholar
- Warner N, Locarnini S. Mechanisms of hepatitis B virus resistance development. Intervirology. 2014;57(3-4):218-224. PubMed | Google Scholar