Factors associated with late presentation for Lassa fever treatment among symptomatic cases in Ondo State, Nigeria
Abiodun Feyikemi Ipadeola, Grace Iyabo Olasehinde, Olayemi Oluseun Akinnola, Olatunji Mathew Kolawole, Adaora Rosemary Ejikeme, Oladipupo Banji Ipadeola
Corresponding author: Abiodun Feyikemi Ipadeola, Department of Biological Sciences, Covenant University, Ogun State, Nigeria 
Received: 24 Jan 2023 - Accepted: 09 Apr 2023 - Published: 17 Apr 2023
Domain: Infectious diseases epidemiology, Public health emergencies, Laboratory medicine
Keywords: Lassa fever, late presentation, onset of symptoms, mortality, Ondo State, Nigeria
©Abiodun Feyikemi Ipadeola et al. PAMJ-One Health (ISSN: 2707-2800). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Abiodun Feyikemi Ipadeola et al. Factors associated with late presentation for Lassa fever treatment among symptomatic cases in Ondo State, Nigeria. PAMJ-One Health. 2023;10:6. [doi: 10.11604/pamj-oh.2023.10.6.39071]
Available online at: https://www.one-health.panafrican-med-journal.com/content/article/10/6/full
Research 
Factors associated with late presentation for Lassa fever treatment among symptomatic cases in Ondo State, Nigeria
Factors associated with late presentation for Lassa fever treatment among symptomatic cases in Ondo State, Nigeria
Abiodun Feyikemi Ipadeola1,&, Grace Iyabo Olasehinde1, Olayemi Oluseun Akinnola1, ![]() Olatunji Mathew Kolawole2,
Olatunji Mathew Kolawole2, ![]() Adaora Rosemary Ejikeme3, Oladipupo Banji Ipadeola4
Adaora Rosemary Ejikeme3, Oladipupo Banji Ipadeola4
&Corresponding author
Introduction: this study assesses the socio-demographic factors associated with late presentation among suspected Lassa fever (LF) cases in Ondo State, Nigeria. Late presentation was determined as presentation to treatment center after sixth day of onset of symptom.
Methods: a cross-sectional study conducted among suspected LF cases who presented at Federal Medical Center, Owo Ondo State, Nigeria. Patient level data from December 2019 to May 2020 was extracted from medical records including socio-demographic variables, test outcomes and treatment outcomes. Descriptive statistics was conducted to measure the distribution of the disease and Chi-Square analyses to determine statistical association while multiple logistic regression analysis was used to identify significant determinants.
Results: of the 992 suspected cases extracted, 332 (33.47%) tested positive for LF with mean age 34.60 (SD-20.0). Owo local government area (LGA) (52.0%) recorded the highest number of positive cases compared to other LGAs. A total of 421 (42.5%) suspected LF cases presented at the treatment center later than the sixth day of onset of symptoms. Location, locality, and outcome of test presentation were significantly associated with late presentation, while cases that presented at the treatment center after the sixth day of onset of symptoms had higher odds of mortality (P<0.001).
Conclusion: residence in rural areas and months of suspicion of LF were associated with late presentation to treatment center in Ondo State. Provision of treatment in rural communities and all year awareness about LF will prevent late presentation, community-based disease transmission and improve quality of care and chances of survival of cases.
Nigeria is one of the West African countries well known for Lassa fever (LF), a zoonotic acute febrile viral illness [1]. It can be transmitted by “multimammate rat”, an indigenous animal in sub-Saharan Africa including Nigeria. This rat specie carries Arenavirus known as the Lassa virus (LASV) which causes hemorrhagic fever in infected persons. Individuals who are infected with this virus present symptoms such as “fever, muscle aches, sore throat, cough, nausea, vomiting, chest and abdominal pain alongside bleeding from the orifices” [2]. However, the virus is mostly asymptomatic in 80% of infected cases [2,3]. Therefore, an accurate diagnosis will require test assays that can detect all existing strains of the virus [4]. Lassa virus is contracted from ingestion of foods/water contaminated with urea and excreta of infected multimammate rat, inhalation of virus particles, or from eating infected rat [2]. Transmission from one person to another person through contacts with blood and sweat of someone who already has the virus has been reported, and transmission is usually common in households or healthcare facilities [5]. Because symptoms of this disease are not specific, there are higher tendencies of transportation of the virus across non-endemic regions, thereby putting unaffected regions at risk of an outbreak and widespread transmission [6]. While symptoms of LF resemble that of malaria and typhoid fever, laboratory diagnosis is performed through “Enzyme Linked Immunosorbent Serologic Assays (ELISA)” [2]. Currently, LF has no approved or known vaccine, but Ribavirin is widely used for treatment (Muse et al. 2020).
Since its discovery over 51 years ago, LF is increasing in transmission with limitations in grounded understanding of the disease and the need for further research to fully address unanswered public health concerns. One area of potential work is in developing LF vaccines, which would be key in curtailing the disease [7]. However, this remains a research gap till date as no studies have presented any preventative remedy to this endemic disease. To this end, infected persons are advised to present early to treatment facilities, so they can receive prompt treatment for better chances of survival [8]. Unfortunately, health seeking behavior remains questionable, especially in Nigerian rural communities where numerous sociodemographic factors interplay and affects the ability of individuals within this group to appropriately make optimum healthcare choices [8]. Lassa fever can be treated if detected early [9]. This will require that potential cases are identified and treated in designated treatment centers across the country. This study therefore aims to identify sociodemographic factors associated with late presentation for treatment among suspected LF cases in Ondo State, to guide appropriate response.
Study design: this was a secondary data analysis to identify sociodemographic factors associated with late presentation for treatment of LF among suspected cases in Ondo State in the 2019 - 2020 outbreak.
Setting: the Federal Medical Center (FMC). Owo is a tertiary health facility in Ondo State, Nigeria, designated for treatment of LF and other epidemic prone diseases. The Integrated Disease Surveillance and Response (IDSR) [10,11] collects data on epidemic prone diseases using case investigation forms during active case search and case management forms for cases that tested positive and received treatment in designated treatment centers.
Participants and data collection: data from this study was collected from the hospital medical records of all patients who were tested and treated for LF between December 2019 and May 2020.
Inclusion criteria: patients who were tested and treated for LF between December 2019 and May 2020.
Variables: 1) variables of interest in this study are categorized as predictor variables and include; a) sociodemographic variables (local government of residence, rural/urban status, name of community, sex, pregnancy status if female, age, occupation, contact with rodent, contact with ill person, travel history); b) laboratory diagnosis variables (including date of sample collection for LF test, date of sample testing, date of result release, LF test result - positive/negative); c) case management variables (including date of onset of first symptom, other symptoms presented - e.g. fever, sore throat, abdominal pain, vomit/nausea, body weakness, headache, diarrhea, bleeding, date first presented in treatment center, date of admission/commenced treatment, date of discharge/death, outcome - dead/alive, other conditions - hearing loss etc); 2) the outcome variables for this study were: a) late presentation (1= if case presented after 6 days of illness and 0 = if case presented on or before 6 days of illness); b) outcome of cases.
Data source: data was extracted from the medical records. A data template containing all required variables of interest was developed in MS Excel and shared with the health facility data manager via email. Data was provided in this MS Excel template after ethical approval and letter of authorization to access data was granted.
Data management and analysis
Quantitative variables and statistical methods: descriptive and explorative data analysis were performed. Sociodemographic, diagnosis, treatment and outcome variables were analyzed for cases presented from December 2019 to June May. Frequency distribution and measures of central tendency of both predictor and outcome variables were generated and displayed using tables and charts as appropriate. Bivariate analysis to examine whether there is an association between the predictor and binary outcome variable. The overall aim of the study was to determine factors associated with late presentation and treatment outcomes in LF management in Ondo State, Nigeria. Binary and multiple logistic regression was conducted with p-value as 0.05 level of significance. Variables with significant association were included in the multiple logistic regression. Data cleaning was conducted in MS Excel, and patient records with missing or incomplete data were excluded before analysis.
Ethics: ethical approval was provided by the Health Research Ethics committee of the Federal Medical Center Owo, Ondo State, Nigeria, and a letter of authorization to access patients´ records. To ensure protection of patients´ records, the data collected excluded patient name or any patient identification data such that the data could not be linked to any case specifically. Data was stored in a passworded computer to prevent unauthorized access.
Participants demographics and description
Description of LF cases by sociodemographic characteristics in Ondo State 2020: from December 2019 to May 2020, total of 992 suspected LF cases were reported in all the 17 LGAs with a mean age 34.60 (standard deviation SD - 20.0). A total of 421 (42.5%) suspected cases presented late at the treatment center with a mean age of 34.09 (SD 20.1). Also, 273 (27.5%) of the suspected cases who presented late at the treatment center were residents of Owo LGA. A total of 256 (25.8%) suspected LF cases who presented late at the treatment center lived in urban residence. Majority of the suspected cases who reported late at the treatment center had symptoms in February 2020 154 (15.5%), January 2020 114 (11.5%). Of all suspected cases, 329 (33.2%) tested positive for LF (Table 1). Additionally, the distribution of LF positive cases across 17 LGAs shows that Owo has the highest proportion of cases 171 (52.0%), followed by Akure South 47 (14.3%), and Ose 34 (10.3%) LGA compared to Idanre and Ile Oluji where no cases were found. The North-Eastern part of Ondo State recorded the highest number of LF cases while the other parts of Ondo State recorded fewer cases. Businessmen/artisans/retired contributed to 39 (11.8%) of positive cases, followed by government/private employee 26 (7.9%). Students in tertiary education level also contributed to 43 (6.6%), followed by those in secondary education level 52 (7.9%).
Outcome data
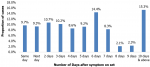
Distribution of suspected cases with respect to number of days between onset of symptom and presentation in treatment center: the average period between manifestation of clinical symptoms and presentation at the treatment center was 5.57 days with standard deviation 5.13 (C.I. =5.25 - 5.89). Of all the suspected cases 15.3% presented for treatment within 10 days or more of onset of symptom while 9.3% presented on same day and 9.7% presented a day after clinical presentation (Figure 1).
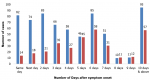
Distribution of tests result with respect to number of days between onset of symptom and presentation in treatment center: the highest proportion of laboratory-confirmed cases was identified among suspected cases who visited the treatment center after six days 58 (40.6%), 10 days and above 57 (37.5%), five days 45 (49.4%) of onset of symptom (Figure 2).
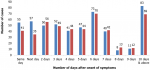
Distribution of number of days between onset of symptom and presentation in treatment center, by sex: a larger proportion of females visited the treatment center between day one and six after manifestation of clinical symptoms, whereas majority of males visited the treatment centers after seven days of symptoms manifestation (Figure 3).
Number of days between onset of symptom and presentation in treatment center, by locality (urban/rural): majority of suspected cases who reported at the treatment center between the day of clinical manifestation and four days after symptoms lived in urban areas. A larger proportion of the rural dwellers were oberved to have reported at the treatment center after five days of onset of clinical symptoms (Figure 4).
Test of association between case presentation and sociodemographic variables: there was a statistically significant association between the LGA of residence and late presentation at the treatment center among suspected cases for LF in Ondo State [Chi-square =213.4, p<.001]. Also, there was a significant relationship between the locality of residence and presentation at the treatment center [Chi-square =55, p<.001] and the outcome of result was statistically significant in relationship to late presentation at the treatment center among suspected LF cases [Chi-square =16.06, p>.001]. Similarly, the month during which suspected LF cases experienced symptoms for LF was significantly associated with the late presentation at a treatment center in Ondo [Chi-square =29.1, p<.001]. In contrast, there was no statistical significance between presentation at the treatment center among suspected LF cases in Ondo State and age group [Chi-square =4.3, p>.001] and between presentation at the treatment center with gender [Chi-square 0.3, p>001] (Table 2).
Late presentation and final outcome: the case fatality rate (CFR) of suspected cases who reported within 6 days and even within 7-9 days at the treatment center following manifestation of clinical symptoms was <1% compared to those who reported 10 or more days after onset of clinical symptoms who had a CFR of 44% (Figure 5).
Chi-square analysis of presentation and outcome: in determining the association between presentation at the treatment center and treatment outcome among suspected cases for LF, there was a statistically significant association as the odds of dying from the illness was 4.2 times higher among suspected LF cases who presented late to treatment center compared to cases who presented early (Chi-square = 14.59, p<0.001, O.R. = 4.2, C.I.: 1.9200, 9.2213).
Determinants of late presentation: the odds of presenting late to the treatment center was 2.89 times higher among rural dwellers compared to urban dwellers [O.R.=2.89 (95% C.I.: 2.15-3,89), p<.0001]. The odds of late presentation at the treatment center were 7.29 higher among suspected cases who developed symptoms in December compared to those who developed symptoms in May [O.R. =7.29 (95% C.I.: 2.99 -17.84), p<0.001], and 2.10 times higher among suspected cases who developed symptoms in April [O.R. = 2.10, C.I.:1.122 - 3.94] compared to those who developed symptoms in May. The odds of presenting late at the treatment center was 1.42 times higher among those who later tested negative to LF [O.R.= 1.42, C.I.; 1.07 - 1.90], compared with those who tested positive (Table 3).
This study assessed the socio-demographic factors responsible for late presentation of suspected LF cases at the treatment center in Ondo State, Nigeria. Socio-demographic variables such as age, sex, educational level, LGA, locality of residence, month of clinical presentation and prior visit to other health facilities were explored for significance. While there are underlying socio-demographic factors that influence health seeking-behaviors and presentation at the health facility during certain illnesses in Nigeria, it was important to assess certain predicting factors as it relates to the late presentation of suspected LF cases to treatment center [8]. Findings from this study reveals that some residence rural locality, negative LF test result, and months of clinical symptoms were associated with late presentation at the treatment centers in suspected LF cases in Ondo State. However, other factors such as age, sex and prior visit to other facility were not statistically associated with late presentation at the treatment center. Additionally, suspected cases who had visited the treatment center late after the onset of clinical symptoms had higher odds of mortality compared to those who visited the treatment center within the first six days.
In this study, it was revealed that almost half of the suspected cases reported late at the treatment center. While there is limited knowledge regarding the burden of delayed clinical visit among suspected LF cases, numerous studies have identified late initiation of ribavirin therapy among LF in endemic regions. Previous studies have reported on late presentation at treatment center and misdiagnosis of LF. In Sierra Leone, out of 36 cases that were confirmed for LF among hospitalized children and women with obstetric conditions, only 35% initiated ribavirin therapy within 6 days after hospital admission [12]. In Liberia, the presentation of mild symptoms led to the misdiagnosis and delayed diagnosis of LF and delayed initiation of treatment among LF cases [13]. In Republic of Benin, a patient was initially treated for other illnesses and was only suspected for LF after persistent fever presentation and diagnosis was confirmed after death of the cases [14]. Although there are no studies assessing the factors responsible for late presentation at treatment center among LF cases, studies across African countries have shown similar burdens of late presentation at clinic and poor health seeking behaviors among individuals seeking care for infectious as well as non-communicable diseases [15,16]. In Nigeria, studies have identified higher proportions of late presentation at the health facility among individuals seeking healthcare for various illnesses [17-19]. In comparison with other studies, presentation at treatment centers for most acute febrile illnesses including LF remains relatively similar due to the non-specific nature of symptoms presented by the group of infectious diseases. As a result, most of the cases are often misdiagnosed as malaria either by affected individuals or the health facilities until these cases become unresponsive to malaria treatment [2,20]. It is therefore important that studies be conducted across LF endemic region to assess the timeliness of case reporting at the treatment center for the diagnosis and commencement of treatment as promptness plays a critical role in the quality of care and chances of survival among LF cases. This can also be assessed by identifying the prevalence of misdiagnosis of LF and how this factor affects diagnosis and initiation of ribavirin therapy.
The role of early diagnosis of LF is critical in ensuring timely identification and confirmation of cases to ensure prompt and effective management of the disease and improve chances of survival. In this study, it was observed that late presentation at the treatment center was associated with increased odds of mortality among suspected LF cases in Ondo State. In Ondo State, the treatment center for LF is in urban region, as a result, proximity becomes a major concern as suspected cases in rural regions may be challenged with the difficulty in accessing the treatment center due to distance and cost of transportation from rural residence. Additionally, place of residence most often determines health seeking behaviors and presentation at the health facility among people seeking healthcare services. In this study, LGA and locality of residence were found to be associated with late presentation of suspected LF cases. Majority of the suspected cases from LGAs away from the treatment center in Owo LGA were less likely to report early for laboratory confirmation and initiation of treatment for the disease. Hence, suspected cases residing in rural regions were less likely to report early to the health facility for initiation of treatment compared to those in the urban regions. These findings have shown relative consistency with other studies within and outside Nigeria that found significant influence of locality of residence on health seeking behavior and late presentation at the health facility [18,21,22].
In Bangladesh, distance to treatment center was found to be associated with health-seeking behavior for infectious diseases [22] while in Nigeria, long proximity was a predictor for late presentation at the health facility among pulmonary tuberculosis patient in rural areas [18]. Also, in Nigeria, breast cancer patients from rural communities were more likely to have poor health seeking behavior and present late at the health facility for care [21]. The location of health facilities within urban regions, which is a major situation in Nigeria, remains a significant predictor of health seeking in rural communities and a lingering public health challenge that needs to be addressed. This study identified a relationship between the month of onset of clinical symptoms and late presentation among suspected cases. This mean that most suspected cases who experienced clinical symptoms during the months of the epidemic may have been likely to report early to the treatment center for laboratory confirmation and treatment. This may be because of the awareness of the community about the seasonality of the outbreak.
However, it is important to re-inform the community as cases are now being identified all year round, especially in Ondo State which is currently one of the epicenters for the outbreak. The burden of late presentation at the treatment center in Ondo State provides a credible justification for why there are an increased number of cases and burden of the disease. As infected individuals remain undiagnosed, communities are at increased risk of transmission and spread of the disease, while the risk of advanced disease and chances of survival in relationship to diagnosis of LF cases continue to worsen. Similar findings have been seen in Sierra Leone, where only 56% of the laboratory confirmed cases-initiated ribavirin treatment within a median duration of 8 days from onset of hospital admission and 87% of individuals who were diagnosed late for the disease died before initiation of ribavirin therapy [12]. Although a study revealed that initiation of ribavirin treatment mitigates the risk of mortality among laboratory confirmed LF cases, treatment with ribavirin is most effective when cases report and initiate early treatment [23]. This means that optimum care for LF and chances of survival is most significantly dependent on early diagnosis and presentation for treatment. The limitation of this study is that the data used for this study was collected by the health facility, hence the authors do not have influence over the data. However, comparison of the results of this study with previous studies findings shows that it can be generalized.
In conclusion, the burden of LF and late presentation at the health facility which is usually affected by health seeking behaviors remains a major public health concern that needs to be addressed in Nigeria, Africa and all Low- and Middle-Income Countries. As it relates to the epidemiology of LF in Nigeria, Ondo State is considered one of the epicenters for the disease outbreak and findings from this study emphasizes the importance of certain factors in ensuring treatment effectiveness, prevention, and control of the disease. Some socio-demographic factors have been shown to influence the diagnosis of the disease and treatment outcomes among individuals suspected for LF within the State. This study provides information on these factors for a targeted response against the disease. Addressing the challenges found in this study would prevent late presentation of suspected LF cases thereby leading to the prevention of community-based disease transmission and spread of the virus while improving the quality of care among LF cases and their chances of survival. This may also be critical in creating more awareness towards seeking early treatment with high index of suspicion among the public.
What is known about this topic
- Nigeria is one of the West African countries well known for Lassa fever;
- Lassa fever can be treated if detected early.
What this study adds
- This study assessed the sociodemographic factors associated with late presentation among suspected Lassa fever (LF) cases;
- Residence in rural areas and month of suspicion of LF were associated with late presentation to treatment center.
The authors declare no competing interests.
All authors contributed to the conception, design, acquisition, analysis, interpretation of data and drafting the article or revising it critically for important intellectual content. They equally read and approved the final version to be published.
We are grateful to all the management and staff of FMC Owo for providing the data for this study.
Table 1: description of sociodemographic characteristics of LF cases in Ondo State, 2020
Table 2: test of association between sociodemographic variables and late presentation
Table 3: output of multivariate logistic regression
Figure 1: distribution of suspected cases with respect to number of days between onset of symptom and presentation in treatment center
Figure 2: distribution of test result with respect to number of days between onset of symptom and presentation in treatment center; blue bar: negative; red bar: positive
Figure 3: distribution of number of days between onset of symptom and presentation in treatment center, by sex; blue bar: female; red bar: male
Figure 4: number of days between onset of symptom and presentation in treatment center, by locality (urban/rural); blue bar: rural; red bar: urban
Figure 5: distribution of outcome with respect to number of days between onset of symptom and presentation in treatment center; N= 280 of 332 (84% of total); blue bar: alive; red bar: dead
- Ilori EA, Furuse Yuki, Ipadeola OB, Dan-Nwafor CC, Abubakar Anwar, Womi-Eteng OE et al. Epidemiologic and Clinical Features of Lassa Fever Outbreak in Nigeria, January 1 - May 6, 2018. Emerging Infectious Diseases Journal. 2019;25(6):1066-74. PubMed | Google Scholar
- Joseph Agboeze, Onoh Robinson, Eze Justus, Nwali Matthew, Ukaegbe Chukwuemeka. Clinical Profile of Lassa Fever Patients in Abakaliki, South- Eastern Nigeria, January - March 2018. Ann Med Health Sci Res. 2018;9:598-602. Google Scholar
- Ejikeme AR, Olajide Lois, Thomas SS, Anueyiagu Chimezie, Aghogho Gbetsere, Akinbiyi Gbenga et al. Characteristics of Lassa Fever Outbreak in Ondo State, Nigeria, Year 2019. East African J Heal Sci. 2021;3(1):115-25. Google Scholar
- Tambo Ernest, Adetunde OT, Olalubi OA. Re-emerging Lassa fever outbreaks in Nigeria: Re-enforcing “One Health” community surveillance and emergency response practice. Infectious Diseases Poverty. 2018;7(1):7-37. PubMed | Google Scholar
- Mariën Joachim, Kourouma Fodé, Magassouba NF, Leirs Herwig, Fichet-Calvet Elisabeth. Movement Patterns of Small Rodents in Lassa Fever-Endemic Villages in Guinea. Ecohealth. 2018;15(2):348-59. PubMed | Google Scholar
- Amorosa Valerina, MacNeil Adam, McConnell Ryan, Patel Ami, Dillon KE, Hamilton Katherine et al. Imported Lassa Fever, Pennsylvania, USA, 2010. Emerging Infectious Diseases. 2010;16(10):1598. PubMed | Google Scholar
- Institut Pasteur. News from the Institut Pasteur 2019. Lassa fever: vaccine set to be trialed. Accessed December 17, 2022.
- Do Mai, Babalola Stella, Awantang Grace, Toso Michael, Lewicky Nan, Tompsett Andrew. Associations between malaria-related ideational factors and care-seeking behavior for fever among children under five in Mali, Nigeria, and Madagascar. PLoS One. 2018;13(1):243-14. PubMed | Google Scholar
- Dhillon RS, Srikrishna Devabhaktuni, Garry RF. Early detection of Lassa fever: the need for point-of-care diagnostics. Lancet Infectious Diseases Journal. 2018;18(6):601-2. PubMed | Google Scholar
- Nigeria Center for Disease Control and Prevention. National Technical Guidelines for Integrated Disease Surveillance and Response. Accessed December 17, 2022.
- CDC. Division of Global Health Protection 2021. Integrated Disease Surveillance and Response. Accessed December 17, 2022.
- Dahmane A, van Griensven J, Van Herp M, Van den Bergh R, Nzomukunda Y, Prior J et al. Constraints in the diagnosis and treatment of Lassa Fever and the effect on mortality in hospitalized children and women with obstetric conditions in a rural district hospital in Sierra Leone. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2014;108(3):126-32. PubMed | Google Scholar
- Woyessa AB, Maximore Leroy, Keller Darius, Dogba John, Pajibo Myer, Johnson Kumblytee et al. Lesson learned from the investigation and response of Lassa fever outbreak, Margibi County, Liberia, 2018: case report. BMC Infect Dis. 2019;19(1):213-98. PubMed | Google Scholar
- Attinsounon CA, Ossibi Ibara BR, Alassani Adébayo, Adé Serge, Saké Khadidjatou, Glèlè-Kakaï Clement et al. Report of a fatal case of Lassa fever in Parakou in 2018: clinical, therapeutic, and diagnostic aspects. BMC Infect Dis. 2018;18(1):185-15. PubMed | Google Scholar
- Luma HN, Jua Paulia, Donfack OT, Kamdem Felicite, Ngouadjeu Eveline, Mbatchou HB et al. Late presentation to HIV/AIDS care at the Douala general hospital, Cameroon: its associated factors, and consequences. BMC Infect Dis. 2018 Jul 3;18(1):298. PubMed | Google Scholar
- Dunyo Priscilla, Effah Kofi, Udofia EA. Factors associated with late presentation of cervical cancer cases at a district hospital: a retrospective study. BMC Public Health. 2018;18(1):14-782. PubMed | Google Scholar
- Awofeso Opeyemi, Roberts AleroAnn, Salako Omolola, Balogun Lanre, Okediji Paul. Prevalence and Pattern of Late-Stage Presentation in Women with Breast and Cervical Cancers in Lagos University Teaching Hospital, Nigeria. Niger Medical Journal. 2018;59(6):74. PubMed | Google Scholar
- Ukwaja KN, Alobu Isaac, Nweke CO, Onyenwe EC. Healthcare-seeking behavior, treatment delays and its determinants among pulmonary tuberculosis patients in rural Nigeria: a cross-sectional study. BMC Health Serv Res. 2013;13:25. PubMed | Google Scholar
- Ibrahim NA, Oludara MA. Socio-demographic factors and reasons associated with delay in breast cancer presentation: a study in Nigerian women. Breast Journal. 2012;21(3):416-8. PubMed | Google Scholar
- Baba Marycelin, Logue CH, Oderinde Bamidele, Abdulmaleek Hauwa, Williams Joshua, Lewis James et al. Evidence of arbovirus co-infection in suspected febrile malaria and typhoid patients in Nigeria. J Infect Dev Countries. 2013;7(1):51-9. PubMed | Google Scholar
- Ayoade BA, Salami BA, Agboola AJ, Tade AO, Adekoya AO, Olatunji AA et al. Beliefs and practices associated with late presentation in patients with breast cancer; an observational study of patient presenting in a tertiary care facility in Southwest Nigeria. African Journal of Cancer. 2015;7(4):178-85. Google Scholar
- Khan MS, Ani JannatulFerdous, Rani Bithika, Apon ShafaetJamil, Rashid Fahmida, Yead TanjilIslam et al. Healthcare-seeking behavior for infectious diseases in a community in Bangladesh. International Journal of Advanced Medical and Health Research. 2018;5(2):52. Google Scholar
- Buba MI, Dalhat MM, Nguku PM, Waziri Ndadilnasiya, Mohammad JO, Bomoi IM et al. Mortality Among Confirmed Lassa Fever Cases During the 2015-2016 Outbreak in Nigeria. Am J Public Health. 2018;108(2):262. PubMed | Google Scholar